Avero Diagnostics and AMLo Biosciences announce the publication of a large-cohort international validation study, confirming that the combined biomarkers, AMBRA1 and loricrin (AMBLor histochemical test) can be used to reliably stratify stage I and II melanomas at genuine low risk of progression. Clinically, this provides additional prognostic information and can help relieve patient anxiety. It may also support a reduction in further invasive diagnostic procedures, lengthy follow-up or unnecessary therapy, lowering the risk of patient complications.
The study results are published in the British Journal of Dermatology.
The retrospective analysis evaluated the clinical value of combined biomarker AMBRA1/loricrin expression in 840 American Joint Committee on Cancer (AJCC) stage I and II non-ulcerated melanoma tissue samples in two distinct cohorts.(1) AMBLor status was compared with up to 12 years clinical outcomes of each cohort. The combined multivariate model showed that the estimated effect of AMBLor was statistically significant with a hazard ratio of 3.469 (p=0.007) and an overall negative predictive value (NPV) of 96.5%.(1) The multivariate analysis of both cohorts also showed significantly reduced recurrence-free survival (RFS) rate in 698 AMBLor-stratified at-risk melanomas compared with 142 AMBLor-stratified low-risk melanomas (RFS 80.4% vs 96.2% p<0.001) independently of Breslow depth.(1) Clinically, this means that AMBLor can reliably stratify melanomas into subcategories of those that are at risk for progression and those that are highly unlikely to progress to advanced disease at the point of excision, according to the companies.
“These robust data from such a large international cohort reinforce the reliability of AMBLor biomarker technology,” says Professor Penny Lovat, Newcastle University Centre for Cancer, chief scientific officer, AMLo Biosciences, and the senior author of the publication. “AMBLor offers accurate, clinically validated, prognostic information relating to tumor progression and will enable physicians to offer reassurance to low-risk patients along with a more personalized approach to disease management.”
Further reading: Can Gene Expression Profiling Guide Melanoma Management?
Predicting Metastatic Melanoma
Only around 20% of patients with early AJCC stage I or II melanomas will progress to metastatic disease but currently there is no accurate predictor for low-risk melanoma recurrence. As a result, disease management guidance recommends the same treatment route and follow-up regimen for all early-stage melanoma patients. Patients may be recommended to undergo sentinel lymph node biopsy to inform subsequent therapy and follow-up options. This is an invasive procedure with potential for complications including seroma, wound infection, lymphedema, and hematoma.(2)
In the U.S. there are gene expression profiling tests available that identify early-stage melanoma patients at high risk of progression, relapse, and death but there is an urgent need for improved early-stage prognostic tests to provide a full risk-profile for melanoma patients. Risk-predication models should incorporate biomarkers for improved accuracy.(3)
“Early evidence suggests that AMBLor can accurately predict low-risk melanomas independent of Breslow depth,” says Gyorgy Paragh, MD, PhD, dermatologist and chair of Dermatology at Roswell Park Comprehensive Cancer Center, Buffalo, New York. “A better understanding of what qualifies as low-risk status in melanoma will not only reassure patients and providers, but in the long term, may also change melanoma management.”
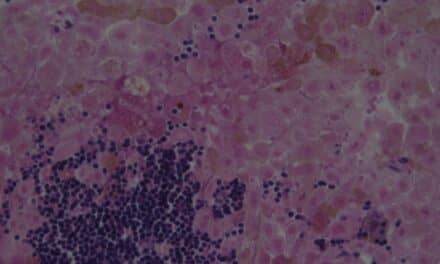
AMBLor technology evaluates protein biomarkers found in the epidermis. In normal skin, these proteins are clearly expressed but original research(4) led Lovat (CSO) found that they are absent or reduced in early-stage cutaneous melanomas that become metastatic and form secondary, often fatal, cancers.
Ryan Fortna, MD, PhD, president of Avero Diagnostics and practicing dermatopathologist, added “I am delighted to see the AMBLor biomarker technology validated on this scale. Incorporating such a simple, reliable, low-cost assay that delivers rapid results into the standard melanoma care pathway can have a large impact on clinical decisions and patient well-being. We believe that widespread implementation of AMBLor could vastly reduce the burden on both individual patients and clinical resources.”
References
- Ewen T, et al. AMBLor as a prognostic biomarker for non-ulcerated early-stage melanoma. Br J Dermatol 2023; In press. https://doi.org/10.1093/bjd/ljad459
- Moody JA, et al. Complications of sentinel lymph node biopsy for melanoma – A systematic review of the literature. Eur J Surgical Oncol 2017;43(2):270–277. https://doi.org/10.1016/j.ejso.2016.06.407
- Kunonga TP, et al. AMBLor as a prognostic biomarker for non-ulcerated early-stage melanoma. BMJ Open 2023;13:e073306. http://dx.doi.org/10.1136/bmjopen-2023-073306
- Ellis R et al, British Journal of Dermatology (2020) 182, pp156–165 https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.18086