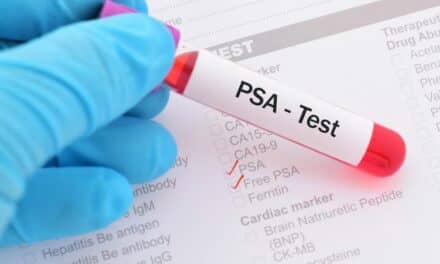
A recent study found that Immunis.AI’s active surveillance blood test for prostate cancer was effective in predicting whether a patient had indolent or aggressive disease.
By Chris Wolski
A prostate cancer diagnosis can have devastating implications for a man’s quality of life. And treatment measures to the diagnosis such as radiation or a prostatectomy can lead to
- Incontinence
- Erectile dysfunction
- Urosepsis or other infections
However, in an increasing number of cases, and because prostate cancer is often slow growing, active surveillance is instead becoming the treatment of choice. This comes with a catch—a yearly exam involves a tissue biopsy. This invasive test is currently the gold standard of active surveillance for prostate cancer.
The result: Only about 30% of men are compliant with regular active compliance involving a biopsy. And lack of compliance has another result.
“The downside of not complying is that the cancer could become aggressive and not curable,” says Geoffrey Erickson, PhD, co-founder and SVP of Corporate Development for Immunis.AI.
Blood-Based Active Surveillance
There is a means to improve compliance, a blood-based cancer surveillance test, which Immunis.AI has developed.
“With a blood test, we know patients would come in,” says Erickson.
The company recently released the results from a prostate cancer risk stratification study evaluating its blood-based liquid biopsy platform, which were published in The Journal of Urology.
The results validate the platform’s ability to accurately stratify risk for patients diagnosed with prostate cancer.
Evaluating the Study Results
The study involved collecting peripheral blood samples from 706 patients with confirmed prostate cancer. According to a company release, immune cells were isolated from these blood samples, and gene expression levels in the patient’s lymphocytes and monocytes were identified using RNA sequencing to evaluate the prostate cancer-specific immune profile of each patient.
To characterize each patient’s immune profile, gene expression levels in their lymphocytes were subtracted from gene expression levels in their monocytes, a process called subtraction-normalization that eliminates the confounding effects of patient-to-patient variability in gene expression levels, according to the company. The AI predictive modeling displayed the normalized immune profile of each patient, which was evaluated against known immune signatures for indolent or aggressive prostate cancer.
The model produced an individual risk score for each patient which categorized them into one of three groups:
- Very low risk (90% NPV)
- Low risk
- High risk
Data from the study shows that the immune profile is effective as a biomarker of prostate cancer severity and is significantly better than clinical factors alone in predicting which patients have aggressive cancer, according to the company.
The study found that the individual risk score accurately established the likelihood of each patient’s cancer being clinically significant and requiring treatment.
Blood Test Availability
Immunis.AI’s surveillance test is not yet available, but the company expects to make it available as an RUO and eventually release it as an LDT. Testing is completed at the company’s Michigan facility.
Chris Wolski is chief editor of CLP.