Widely used biomarkers are not optimal in early detection of liver cancer, the third most common cause of cancer-related death worldwide, according to a new study published in this month’s Gastroenterology.
Two biomarkers used to complement ultrasound in the early detection of hepatocellular carcinoma, or liver cancer, are not ideal, according to Anna S. Lok, M.D., professor of internal medicine at the University of Michigan Medical School and lead author of the study published in the official journal of the American Gastroenterological Association (AGA) Institute.
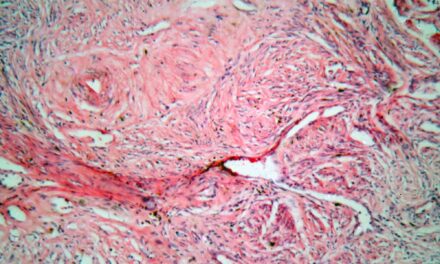
The study analyzed the use of des-gamma-carboxy prothrombin (DCP) and the most widely used biomarker, alpha fetoprotein (AFP). Biomarkers are found in patient’s blood and are used to indicate whether a disease or condition is present.
Liver cancer is the sixth most common malignancy, with 22,620 Americans expected to be diagnosed this year. The incidence of HCC in the United States is increasing and is largely attributed to hepatitis C.
“Most surprising was the finding that patient demographics influenced both des-gamma-carboxy prothrombin and alpha fetoprotein values, but in opposite directions,” said Lok, who also is the University of Michigan’s Alice Lohrman Andrews Research Professor in Hepatology. “This observation merits further investigation, as it might impact the accuracy of these biomarkers in the detection of liver cancer in men versus women and in patients of various races and ethnicity.”
The survival of patients with most malignancies has improved over the last decade, but five-year survival of patients with hepatocellular carcinoma (HCC) has remained less than 10 percent. The poor outcome of patients with HCC is related to late detection with more than two-thirds of patients diagnosed at advanced stages of disease. A major problem with HCC surveillance is the lack of reliable biomarkers. While AFP is the most widely used biomarker for HCC surveillance, experience with DCP is limited.
The study was conducted in 10 centers in the United States and funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
Among 1,031 patients randomized in the Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis Trial, a nested case-control study of 39 HCC cases (24 early stage) and 77 matched controls was conducted to compare the performance of AFP and DCP. Testing was performed on serial serum samples collected during a 12 month period prior to the time of HCC diagnosis.
DCP was not superior to AFP in the early detection of HCC in patients with advanced hepatitis C and neither AFP alone, DCP alone, nor the combination of AFP and DCP was sufficiently accurate to be used for HCC surveillance. The combination of both markers enhanced the sensitivity, indicating that these two markers are complementary. Therefore, prospective studies should be conducted to determine if combining both markers will improve the detection of early HCC and to establish the optimal cutoff values that should be used for patient recall and further testing.
“Until better serum markers are available, ultrasonography remains the preferred tool for HCC surveillance. However, reliable biomarkers to complement ultrasound may improve the detection of early HCC in clinical practice where interpretation of ultrasound is variable,” says Lok. In this study, diagnosis of early HCC was triggered by surveillance ultrasound in only 58% of patients.
Source: University of Michigan Health System