Cancer-detection tests are being developed that not only find the presence of cancer, but identify the organ affected and even the treatment that will be the most effective for a particular patient. Here, CLP takes a look at some of the newest tests available for detecting cancer and what the future holds for cancer diagnostics.
Tumor markers are substances normally present in small amounts in the blood or other tissues. When the amount of these substances rises above normal, cancer might be present in the body. Examples of biomarkers include CA 125 (ovarian cancer), CA 15-3 and 27-29 (breast cancer), CEA (ovarian, lung, breast, pancreas, or gastrointestinal-tract cancer), and PSA (prostate cancer).
Many tests can assess the health of different organs and systems in the body, and if cancer is present, it will usually produce a specific protein in the blood that can serve as a marker for the cancer. Carcinoembryonic antigen (CEA) may be used to determine if cancer has spread to other areas of the body.
Some physicians rely on markers as an early indicator of disease progression or recurrence, with the hope of finding a local, curable tumor. An elevated marker may prompt a physician to check that marker periodically to assess response to chemotherapy. However, a test that registers normal does not prove that a patient is cancer-free, nor does an elevated test necessarily indicate the progression or recurrence of cancer. While they may help along the road to diagnosis, the use of markers to find metastatic cancer has not yet translated into better survival, for example, for women with breast cancer. These tests can also be quite costly.
And since genetics can account for significant variability in drug disposition and effects, microarray-based diagnostic tests are increasingly seen as a solution because they can potentially detect diseases and predict the effects—both positive and negative—of drugs developed to treat them.
For the past 20 to 25 years, tumor markers have been used either as screening tests or as prognosis indicators of tumor recurrence, says Martin Fleisher, PhD, chairman, Department of Clinical Laboratories, and chief, Clinical Chemistry Service, Memorial Sloan-Kettering Cancer Center. Most tumor markers are products of cancer-cell elaboration or the result of the body’s response to a cancer. The tumor markers circulate in the blood as, for example, proteins or glycoproteins.
Early Detection
According to Dean E. Brenner, MD, Kutsche Family Memorial Professor of Internal Medicine and Professor of Pharmacology, University of Michigan Comprehensive Cancer Center, early detection can be accomplished in many ways. For example, there is a procedure for prognosis in breast cancer, the gene chip, which is now commercially available. He says this procedure is controversial as a clinical test because of concerns regarding overfitting. For breast cancer, it’s a microarray (genome chip) test; that is, a way of testing a sample of cells to find out what genes are expressed and what genes are not expressed in that sample. This eventually will allow researchers to learn in much greater detail the exact makeup of the various cells they are interested in, and involves sending tumor tissue to a lab and getting a profile back. Although it’s been a research tool for a while, Brenner says he’s not sure if diagnostic labs would use it, and it’s not universally accepted because of the small size of the samples it uses.
Brenner also notes that some breast cancers make an abnormal amount of Her-2/neu protein, which helps to drive the growth of the cancer. Her-2/neu is expressed on the surface of a cell. Cancer cells express the protein, which can be detected using immunohistochemical methods. Commonly used in pathology labs, this is not at all new. The epidermal growth factor (EGFR) is another immunohistochemical test used to determine whether patients with lung cancer and perhaps other cancers should receive treatment with EGFR ligand binders (antibodies or intracellular targeted inhibitors of EGFR receptor activation). To date, the clinical data are mixed. “Some trials suggest that immunohistochemical detection of EGFR predicts clinical benefit from these new cancer treatments; others do not. So the jury is out on this one,” Brenner says.
Other Detection Methods
Stool DNA markers are exact in detecting cancer early, although the tests are so expensive as to not be cost-efficient, and the results do not represent a huge improvement over the current standards. However, this could be a building block for future improvements. Stools are shipped to labs for analysis and put through a mechanized polymerase chain reaction (PCR), a method for the amplification of DNA. It is an exciting tool, but the cost makes the test impractical, Brenner says. Large quantities have to be collected and shipped to a central laboratory to be analyzed. The method relies upon a high-throughput PCR technology with magnetic bead extraction of key DNA fragments that might contain the mutated DNA sequence associated with a colon neoplasm.
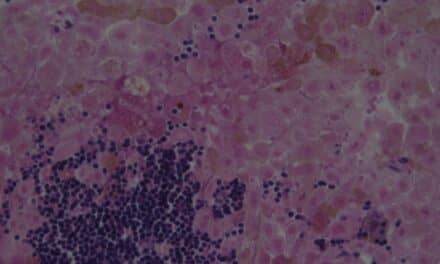
The newest detection methods distinguish between serum and soluble tumor markers that are present in body fluids. They’re primarily serum markers, possibly because molecular or cellular markers use tumor cells instead of bodily excretions, says Erasmus Schneider, PhD, research scientist, Wadsworth Center, director, Oncology Section, Clinical Laboratory Evaluation Program, New York State Department of Health, and associate professor, Department of Biomedical Sciences, School of Public Health, State University New York, Albany. Serum markers are measured by clinical chemistry labs using mostly automated immunoassays. In contrast, with cell-based or molecular markers, the test method of choice is the PCR, wherein DNA is analyzed using an amplification reaction. While these are fairly distinct technologies, both have their clinical utility. Serum markers traditionally have been used to monitor response to therapy, with PSA also for screening. Molecular markers are useful in confirming a diagnosis and measuring residual disease, primarily in leukemia and lymphoma.
“Most tests start with blood, but with serum. Cells are removed from the blood, and with the molecular methods, cells are isolated from the blood. The serum method gives results in about 30 minutes; the molecular method takes about a day to yield results,” Schneider says. These tests have become quite routine, he says. There’s an evolution—but not a revolution—happening in cancer diagnostics. One such evolution is multiplexing, in which several markers are analyzed in parallel using technologies such as Luminex™. The Luminex™ liquid array multiplexing assay system is a bioassay-detection system that can perform up to 100 immunoassays at a time using many small microscopic beads coated in 100 different colors, one for each antibody. A laser instrument can detect the bead’s color and reaction. This method started to get some traction, Schneider says, but it will come into greater use in the future because it offers multiplexing for both serum and molecular markers.
The first tumor marker that received high notoriety was CEA, a glycoprotein that was thought to detect colorectal cancer in its early stage, Fleisher says, but that balloon burst. CEA was the focus of much attention in the early 1970s. “We worked hard to build our own CEA assay by raising antibodies to CEA extracted from metastatic liver cancer. There were no commercially available kits. After several years of testing the clinical sensitivity of CEA, it became apparent that CEA could not be used to detect early colorectal cancer. We bundled CEA with other tumor markers and enzymes to help increase clinical sensitivity. And thus, tumor-marker panel testing was invented. The tumor-marker assays were meant to specifically demonstrate the presence of cancer in the liver, breast, colon, or any other organ.
|
“The problem was that these were broad markers that weren’t very specific,” he says. “A specificity rate of 85% thrilled us.” Over the years, assays improved technically and enabled the measurement of smaller concentrations of biomarkers in the blood. Then, PSA came along—“a home run,” Fleisher says. PSA was the first tumor marker that was approved by the US Food and Drug Administration (FDA) for screening for prostate cancer.
A Golden Age of Tumor Markers
Fleisher says that was “the golden age of tumor markers. We measured tumor markers in urine and spinal fluid. These had good clinical utility, especially spinal fluid, because spinal fluid turns over every 8 hours, lending a kinetic characteristic to tumor markers. We worked on bundling together a battery of tests to make them more specific, and we analyzed every type of fluid, such as breast-cyst fluid, looking for markers that would tell us which women were at risk for breast cancer. We compiled an enormous amount of data, but it wasn’t enough to convince oncologists, who often didn’t want to know this information because there was nothing they could do with the data in terms of patient treatment.” Technology had gotten ahead of treatment, he says. “That was a problem, and we didn’t want to create a medical conundrum for clinicians with data they couldn’t act on.”
So the tests were used for prognosis, not diagnosis—to tell physicians if the treatment was successful. Fleisher says he still gets calls every day from physicians asking, “What do these patients’ results mean? What do I do about an elevated result?”
The tumor-marker results can be used to tell a clinician that treatment is either effective or not. New technology permits the measurement and isolation of circulating cancer cells in the peripheral blood. If cancer cells are present in peripheral blood, they are probably looking for a place to metastasize, he says, and the FDA has approved this assay for measurements in breast-cancer patients. Similar work is also being done with prostate cancer.
Biomarker analysis provides indirect information about the genes that control the growth or death of cancer cells, and it helps determine which genes are on and which are off. “We know what the composition is of the human genome, so we’re busy looking at genes associated with cancer as well as with other genetic and metabolic diseases,” Fleisher says.
Cancer therapy has also changed. Chemotherapy kills both cancer and healthy cells, so therapy is targeted at cancer cells that have faulty growth switches. “We just need to know that the patient has cancer, and we can then focus targeted therapy on cancer, not on healthy cells. It’s like treating an infection with antibiotics. We don’t always know where the infection is before antibiotic treatment, and it’s the same with cancer and targeted therapy. Now, we really just want to know whether cancer is present, not where it is. We used to use tumor-specific markers; now, we just want biomarkers,” Fleisher says.
He says the most debatable and controversial new technique for biomarker discovery is proteomic analysis. Proteomic analysis is the study of protein structure (molecular size and charge). It measures a patient’s proteomes (the complement of proteins expressed by an organism, tissue, or cell type) for specific diseases, based on the pattern of proteins found in serum. Most data published on proteome analysis is clinically unreliable, Fleisher says. Just 2 years ago, it was announced with great fanfare that this method could detect ovarian cancer, and labs jumped in and offered the test to physicians, but “it was premature and unreliable,” he says. “We began to look at the basic science of what happens to proteins in the blood of cancer patients. What is the effect of specific proteinases produced by specific cancers? There are many questions and much work to be done. Claims for proteome analysis have not stopped, but they are less pretentious,” Fleisher says.

Brenner sees many radical diagnostic tools in development, such as risk-profiling in genes in patients’ white blood cells, gene chips, and protein-expression profiles. Antibody assays use small samples, allowing protein arrays—that is, interrogation of many proteins—instead of single-protein assays. Some technologies use larger platforms, but these are still microanalytic tools, he says. “Interrogating specific groups of genes will be quantitatively better using gene expression, rather than direct gene technology,” he says. Gene expression uses fragments of genes and expresses them to detect protein products. The protein product is detected and quantitated using mass spectroscopy to determine the molecular weight of a substance. “This will evolve into a clinical tool,” Brenner says, as it also detects protein profiles from cells and tissues for diagnostics. This represents an evolution of genetic detection—from determining how amplified RNA binds to a set of oligonucleotides on a chip to interrogating proteins translated directly from gene fragments extracted from human biosamples using mass spectroscopy. Although it is still in development, Brenner says the method is now being rapidly adapted to clinical and diagnostic use. Also, some genetic tests are being used, such as epigenetic tests, which detect gene silencing without an associated mutation of the DNA. These tests can determine how genes are turned off and on.
The main development for the future is translating genes to get protein profiles. In such a system, messenger RNA is obtained from a DNA fragment in a human sample to create an expression system to get clean proteins to detect and to quantify. The evolution of mass spectroscopy from a research to a clinical tool can identify genes’ expression products that are risk fingerprints. The ability to link these technologies will be key for the future, Brenner says.
Schneider sees more and better screening for cancer in the future. Current technology presents too many false positives, he says. “Screening has to become more specific. Also, I feel we’ll use three or four markers together instead of just one. Each by itself may not be good enough, but together they are.”
He also sees more predictive and/or prognostics testing, where multiplex tests will predict how a patient will react to certain drugs or treatments, and which ones might be more effective. For example, Genentech offers a treatment for breast cancer that works only in about 30% of women and must be used in conjunction with a test to see if the patient is compatible with it. “We’re moving toward more predictive ways to treat cancer,” he says. An extension of this is pharmocogenomics, which gives some advance idea of which treatment may be effective. “This gives doctors an advantage,” he says, “because they don’t waste time treating with a drug that doesn’t work. On average, cancer drugs work only in approximately 50% of patients; however, if we could identify those 50% up front, we could spare the other 50% what can be unpleasant treatments that won’t work on them anyway.”
The pharmaceutical industry has come to realize that, rather than fight the trend to preselect patients, it is better off embracing it. This was originally seen as a loss of revenue, but the companies now see the long-term savings, he says. For one thing, this also means more lab work. There’s been a clear change over the past 5 or 6 years.
Schneider says microarrays, a highly multiplex platform that can measure thousands of markers instead of just five or six, is a great research tool, but it won’t make it to diagnostics in its present form. “I’m skeptical, because compared to standard tests, the technology is challenging both from a quality-control standpoint for the manufacturers and in practice in the lab. Also, do we really need to test that many markers? The consensus is that 50 to100 markers are enough,” Schneider says. One company’s version measures 70 markers. With new, targeted therapies, “we measure before we treat,” Schneider says. “Targeted drugs target specific molecules, which allows us to target treatment.”
The Dream: One-Drop Detection
“We want to be able to take a small drop of blood from a patient, analyze it, and determine if they have cancer. That could happen in 10 years or less,” Fleisher says. The methods used today are only 10 or 15 years old. “We’ve come a long way and have become specific in assigning certain genes to certain diseases. In the next 10 to 15 years, an explosion of technology will assist the clinician in patient management.
“We’re learning a lot about genes as we use genomic analysis to see what drugs work and which can actually be harmful to the patient. Pharmacogenomics is tremendously important, as is cytogenetics (determining which genes are on and which are off). The older concept of measuring markers that circulate in the blood is still being used, but some may become a thing of the past.”
Gary Tufel is a contributing writer for Clinical Lab Products.