Current challenges of treating long COVID are amplified by a lack of consensus on what constitutes long COVID and lack of formal diagnosis methods, which is further exacerbated by limited research data of varying quality and consistency, according to a new report.
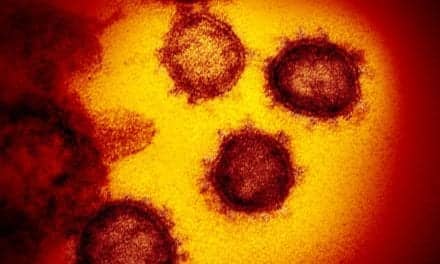
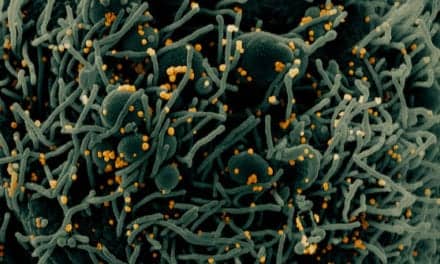
Early reports foretell a difficult challenge with long COVID, which researchers call Post-Acute Sequelae of SARS-CoV-2 infection (PASC). Some patients with prior acute COVID-19 cases have continued to report new or persistent health issues affecting nearly every organ system, further impacting the ability to reach a diagnosis consensus of long COVID.
Researchers from UCLA Health and the David Geffen School of Medicine at UCLA, with a colleague at the University of Washington in Seattle, point out that while PASC has been approved for inclusion and protections within the Americans with Disabilities Act, which has strict medical and legal paperwork requirements, there is limited study data or medical consensus on what constitutes long COVID and its diagnosis. Report writing was published in the Annals of Internal Medicine.
“The first challenge when studying any disease is knowing how to diagnose it, and although we have seen serious medical consequences stemming from COVID-19, we do not yet have definitive diagnostic criteria,” says Lauren E. Wisk, PhD, a researcher with the Division of Internal Medicine and Health Services Research in the David Geffen School of Medicine at UCLA and the UCLA Fielding School of Public Health, the article’s first author. “We believe that as more high-quality data emerges, the current list of symptoms will become better refined, and the timing and duration of symptoms will become clearer. So far, however, these have remained elusive.”
Although multiple studies are in progress for long COVID diagnosis, the authors say making useful comparisons across studies are nearly impossible without a consensus on uniformly applied criteria.
“We need high-quality data and information that supports an accurate diagnosis before patients can receive appropriate supportive care and effective, disease-specific therapy,” says Joann G. Elmore, MD, MPH, professor at the David Geffen School of Medicine at UCLA and the UCLA Fielding School of Public Health, the article’s senior author. “The scientific research community will need to be able to provide data that helps the medical community to distinguish long COVID symptoms from those of other illnesses.”
The report authors also point out that researchers of long COVID must contend with confounding issues in study design that can skew results, such as biases that can result from patient’s own recollection and clinicians’ interpretation of symptoms.
“Due to the dynamic nature of the virus itself and the technology available to test, monitor, and treat infection, substantial variation may exist in apparent clinical presentation of PASC,” the authors write. “Now more than ever, we must implement robust, standardized, longitudinal assessments of health and well-being across systems and settings, including premorbid evaluation, to facilitate real-time monitoring of trends.”
In addition to recall and surveillance bias, study selection bias and healthcare access could produce misleading results for the consensus to diagnose long COVID, according to the article.
“People who were already vulnerable to socioeconomic and racial or ethnic disparities – people who often have limited access to health care – have disproportionately borne the burden of the COVID-19 pandemic. Now, inequities in the development, presentation and documentation of long COVID-19 may also be accentuated,” says Wisk.
The authors offer potential solutions to ensure equity in future study and treatment, first urging the medical community to come together on a case definition that can be consistently applied. They further recommend that researchers implement robust and standardized measures of potential risk factors and outcomes; consider risk of bias when designing studies; take steps to facilitate cross-study comparisons; and to “be judicious in application of this evolving evidence as we all strive to provide effective and efficient care that reduces prior inequities.”