By Monica Herrera, MD, and Jennifer Walker
The University of Arizona began monitoring campus wastewater for evidence of SARS-CoV-2 in March of 2020. That August, a sample from one of their 20 on-campus dorms revealed a viral load—an indication that individuals living in that residence might be infected.1 The school tested each of the 311 residents in that dorm and found two positive cases—neither was yet exhibiting symptoms, suggesting they could have passed the virus silently throughout the student population had they not been found in time. Instead, they were isolated before they could infect others, and the school averted a wider outbreak.
This example is just one of many where wastewater testing—a strategy that has been used for decades by epidemiologists to track disease outbreaks—is being used to predict and stem the spread of SARS-CoV-2. And now, epidemiologists have access to a technology that gives them a clear picture of SARS-CoV-2’s presence in wastewater: droplet digital PCR (ddPCR).
Wastewater testing is possible because many viruses and various metabolites pass through our bodies and into our sewage. For many infectious diseases, wastewater testing is not only more efficient than clinical testing, but it also has the potential to measure the scale of an outbreak more accurately by detecting asymptomatic or presymptomatic carriers. Prior to covid-19, the method had been deployed to help identify norovirus and poliovirus in wastewater, in the absence of clinical cases.2
Early reports suggest that SARS-CoV-2 can be detected this way as well—because the virus binds to angiotensin-converting enzyme 2 (ACE2), which is abundant in the small intestine, and sloughs off into feces.3
Because of the urgency of the covid-19 pandemic, many universities, municipal water treatment plants, and other organizations are rapidly deploying ddPCR technology to detect SARS-CoV-2 in local wastewater. The state of Michigan, for example, is adopting ddPCR technology at 18 institutions to monitor wastewater for the virus and aid in slowing its spread.4
While the long-term impact of this strategy is not yet known, several organizations around the United States are already showing good results. At the Hampton Roads Sanitation District (HRSD) in Virginia, for example, Raul Gonzales, PhD, and his team demonstrated that ddPCR-based quantification of SARS-CoV-2 concentration in wastewater correlates with spikes in covid-19 cases in the community.5
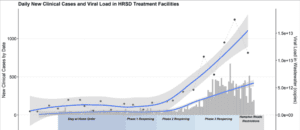
The district encompasses approximately 3,100 square miles, with a population of 1.7 million. Combined, the 16 HRSD service plants process 249 million gallons of wastewater per day. In early March 2020, the team began collecting 1-liter samples of wastewater from HRSD’s nine major plants. They detected SARS-CoV-2 RNA in raw wastewater from the region every time they tested it—even during the first week of sampling, when the region had only two diagnosed clinical cases of covid-19. Viral load remained low during the first 2 weeks of sampling and then increased until mid-April.

Because samples were taken from nine different treatment plants spread across the region, the team was able to correlate viral load with the geographic distribution of clinical cases. This data showed that while increased clinical testing reveals more covid-19 cases, that increase was not uniform across their catchment area. This study demonstrated that testing wastewater with ddPCR technology as the pandemic fluctuates in size could help direct clinical resources to where they will be needed most. Viral load also correlated with specific government actions: It leveled off following Virginia’s statewide shutdown order and then increased dramatically during its phased reopening (Figure 1).

Wastewater testing is not a substitute for individual testing. But it is a relatively simple way to monitor a community’s susceptibility to an outbreak and inform actions to stop the spread of the virus. As seen throughout the United States, wastewater testing can be used to target resources to areas that are most susceptible to a rise in covid-19 cases and allow authorities to act to prevent the spread of the virus. ddPCR’s high sensitivity allows scientists to detect very low viral concentrations in wastewater and potentially identify local outbreaks in the earliest stages. More widespread use of wastewater testing will hopefully help everyone stay alert and do what they can to stay safe.
Monica Herrera, MD, is program head for human genetics and infectious disease in the Digital Biology Group at Bio-Rad Laboratories.
Jennifer Walker is director of marketing programs for Bio-Rad’s Digital Biology Group.
This article was originally published as a sidebar to The Race for an Ultrasensitive Coronavirus Test.
References
- Pineda P, Leingang R. University of Arizona wastewater testing finds virus at dorm, prevents outbreak. Arizona Republic. August 27, 2020. Available at: https://www.azcentral.com/story/news/local/arizona-education/2020/08/27/university-arizona-covid-19-outbreak-prevented-dorm-wastewater-testing/5649579002/. Accessed January 5, 2021.
- Tang A, Tong Z-D, Wang H-L, et al. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. 2020;26(6):1337–1339. doi: 10.3201/eid2606.200301.
- Kitajima M, Ahmed W, Bibby K, et al. SARS-CoV-2 in wastewater: state of the knowledge and research needs. Sci Total Environ. 2020;739:139076. doi: 10.1016/j.scitotenv.2020.139076.
- Michigan Department of Environment, Great Lakes, and Energy. Michigan launches $10 million covid-19 in wastewater surveillance grant program. September 16, 2020. Available at: https://www.michigan.gov/egle/0,9429,7-135–539750–,00.html. Accessed: January 5, 2021.
- Gonzalez R, Curtis K, Bivins A, et al. Covid-19 surveillance in Southeastern Virginia using wastewater-based epidemiology. Water Research. 2020;186:116296. doi: 10.1016/j.watres.2020.116296.





