The role of rapid testing in reducing HAIs
By Jonathan Cooke, PhD, and Jayne Ellis, PhD
Healthcare-associated infections (HAIs) are becoming increasingly urgent global concerns, killing more people each year than AIDS, flu, and traffic accidents combined, and incurring spiraling healthcare costs.
The incidence of HAIs has been rising. Just this year, there was a medical device-related outbreak of carbapenem-resistant Enterobacteriaceae (CRE) infection at Ronald Reagan UCLA Medical Center. This alarming trend has mirrored the increased rates of resistance to antibiotics. Studies indicate that 30% to 50% of antibiotics prescribed in hospitals are unnecessary or inappropriate, and this overuse of antibiotics has been a significant driver of the growing incidence of HAIs, namely Clostridium difficile and Methicillin-resistant Staphylococcus aureus (MRSA). In fact, the overuse of antibiotics is especially prevalent in hospitals, where broad-spectrum antibiotics are often prescribed for reasons of expediency in place of targeted narrow-spectrum therapies.
C. difficile is the most common cause of healthcare-associated diarrhea in industrialized countries, and it has become the most common HAI in US hospitals, causing almost half a million infections among patients in a single year. C. difficile is present in 13 of every 1,000 hospital inpatients in North America, contributing to the estimated annual economic burden of approximately $3.2 billion. The single most important risk factor for C. difficile infection is antibiotic use.1
Worldwide, it is estimated that up to 53 million people carry MRSA bacteria, and rates are increasing rapidly. This makes MRSA the most commonly identified antibiotic-resistant pathogen in Europe, the Americas, North Africa, the Middle East, and Asia. This ever-increasing rise is especially concerning because patients infected with multidrug resistant organisms such as MRSA are likely to have longer and more expensive hospital stays, and may be more likely to die as a result of the infection. Vancomycin is often the last line of defense against MRSA, and its continued overuse makes it inevitable that resistance will emerge. Vancomycin-resistant MRSA has already been reported in some countries.2,3
RAPID DIAGNOSTICS UNDERUTILIZED
Although many hospitals and clinics have implemented antimicrobial stewardship programs to help curb the overuse of antibiotics that contributes to C. difficile and MRSA, an important and proven strategy is frequently underutilized: the use of rapid diagnostics that empower healthcare professionals to identify cases when antibiotics should be prescribed and when they can be withheld (see Table 1).

Table 1. Rapid diagnostic tests available for common healthcare-associated infections. Availability varies by market. Click to enlarge.
It is essential that C. difficile and MRSA infections be identified as early as possible, and that steps are taken to ensure the correct treatment is implemented. The latest guidelines for screening C. difficile recommend an algorithmic testing approach that uses glutamate dehydrogenase (GDH) tests or molecular technology to detect infection, and uses a sensitive toxin A/B test to confirm disease. Hospitals should therefore deploy tests that detect GDH and toxin A/B simultaneously; today, there are tests available that do so in as little as 30 minutes.4,5
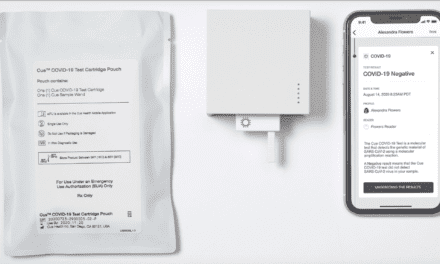
Rapid MRSA testing helps reduce the empirical use of vancomycin and facilitates cost-effective decisionmaking for optimal patient management. A new test that uses monoclonal antibodies can assist in the detection of MRSA directly from bacterial isolates in 5 minutes. In a recent study, a rapid immunochromatographic MRSA assay that provides results at least 1 day sooner than standard antimicrobial susceptibility tests measurably improved treatment regimens for patients with S. aureus infections.6,7
EUROPEAN INITIATIVES
Rapid testing has proven to be a vital and effective aspect of antimicrobial stewardship, as demonstrated by the numerous European countries that have implemented successful initiatives around the importance of diagnostics. Studies from these countries have linked antimicrobial stewardship, infection control, and enhanced routine testing to decreased rates of C. difficile, and reductions in total antibiotic use. (For more information, see the companion article, “A Handlist of Sources on Rapid Testing and HAIs.”)
In the UK, testing has led to a reduction of antibiotics that cause C. difficile by 50% and a subsequent 70% decrease in C. difficile cases. Other successful initiatives include the EU’s ABS International, which focused primarily on hospital-based stewardship efforts; Sweden’s Strategic Program against Antibiotic Resistance initiative, focusing on diagnostics; and France’s social marketing campaign, Keep Antibiotics Working, which targeted both general practitioners and the general public.8–11
Rapid diagnostics offer important benefits beyond their role in reducing HAIs. They address a significant drawback of culture-based testing methodologies, which are sensitive and low cost, but can result in delays of up to 4 days because they rely on growing the bacteria or viruses. During this delay there is a risk for transmitting antimicrobial-resistant organisms to multiple patients.
With the advent of newer, more accurate and rapid diagnostics, these time frames can be reduced dramatically. For example, new technologies can dramatically reduce reporting times from several days to only minutes. This means that healthcare professionals can administer the right treatment sooner, improving patient outcomes and reducing the significant healthcare costs associated with treating disease complications.
STEWARDSHIP
While advances in rapid diagnostics have played a key role in reducing inappropriate use of antibiotics, education needs to keep pace to maximize the utility of these new testing platforms. Hospital personnel have an important role to play in reducing the overuse of antibiotics. Since both laboratory and point-of-care diagnostics are critical if we are to achieve effective diagnosis, monitoring, and treatment of antibiotic-resistant organisms, professionals in both of these areas should work together to maximize their impact. The skills and expertise of laboratory personnel, for instance, can be very effective in the implementation and support of point-of-care diagnostics in a variety of settings.
To help support this important professional education, the Alliance for the Prudent Use of Antibiotics has partnered with Alere, a leading company that develops near-patient diagnostics, on “Test, Target, Treat,” an antimicrobial stewardship initiative that provides tools and diagnostic strategies to support clinicians and increase global awareness of antibiotic resistance and effective interventions.
Antimicrobial stewardship programs in hospitals that address the importance of diagnostics prove to be a critical strategy for reducing antibiotic resistance and HAIs. As rapid diagnostic test technology continues to improve, education on testing continues to be crucial in ensuring best practices in antimicrobial stewardship are followed in US hospitals, and throughout the world.
Jonathan Cooke, PhD, is honorary professor of pharmacy at the University of Manchester Pharmacy School (UK). Jayne Ellis, PhD, is medical director for Western Europe and Nordics at Alere Inc. For further information, contact CLP chief editor Steve Halasey via [email protected].
REFERENCES
- Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372(16):1539–1548; doi 10.1056/nejmra1403772.
- Grundmann H, Aires-de-Sousa M, Boyce J, Tiemersma E. Emergence and resurgence of meticillin-resistant Staphylococcus aureus as a public health threat. Lancet. 2006;368(9538):874–885; doi:10.1016/S0140-6736(06)68853-3.
- Howden BP, Davies JK, Johnson PDR, Stinear TP, Grayson ML. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev. 2010;23(1):99–139; doi: 10.1128/CMR.00042-09.
- Updated guidance on the diagnosis and reporting of C. difficile [online]. London: UK Department of Health, 2012. Available at: www.gov.uk/government/uploads/system/uploads/attachment_data/file/215135/dh_133016.pdf. Accessed June 10, 2015.
- Swindells J, Brenwald N, Reading N, Oppenheim B. Evaluation of diagnostic tests for Clostridium difficile infection. J Clin Microbiol. 2010;48(2):606–608; doi: 10.1128/JCM.01579-09.
- Lodise TP, McKinnon PS. Clinical and economic impact of methicillin resistance in patients with Staphylococcus aureus bacteremia [abstract]. Poster presentation at International Conference of Antimicrobial Agents and Chemotherapy (San Diego: September 2002). Diagn Microbiol Infect Dis. 2005;52(2):113–122; doi:10.1016/j.diagmicrobio.2005.02.007.
- Barrett HL, Trienski TL, DiPersio JR. Proof source: laboratory use of a rapid PBP2a immunochromatographic assay: efficacy and clinical impact [abstract]. Presented at the American Society of Microbiology general meeting, (San Francisco: June 16-19, 2012). Available at: www.alere.com/content/alere/us/en/product-details/pbp2a.html.html 2012.
- Edgar T, Boyd SD, Palamé MJ. Sustainability for behaviour change in the fight against antibiotic resistance: a social marketing framework. J Antimicrob Chemother. 2009;63(2):230–237; doi: 10.1093/jac/dkn508.
- Goossens H, Guillemot D, Ferech M, et al. National campaigns to improve antibiotic use. Eur J Clin Pharmacol. 2006;62(5):373–379.
- Huttner B, Harbarth S. “Antibiotics are not automatic anymore”—the French national campaign to cut antibiotic overuse. PLoS Med. 2009;6(6):e1000080; doi: 10.1371/journal.pmed.1000080.
- Allerberger F, Lechner A, Wechsler-Fördös A, Gareis R. (2008). Optimization of antibiotic use in hospitals: antimicrobial stewardship and the EU project ABS international. Chemotherapy. 2008;54(4):260–267; doi: 10.1159/000149716.