
It doesn’t matter which comes first, a clinical laboratory will not be able to properly function without both a laboratory information system (LIS) and a billing solution. “They go hand in hand,” says Sandy Laughlin, LabDAQ product manager, CompuGroup Medical Inc, Boston. “You can’t run a lab and not get paid for it because you won’t be around for long. But if you’re not running the tests, the billing system alone is useless too.”
The right systems properly integrated can help a laboratory to improve collections, ensure compliance, save time, increase efficiency, and grow volume without adding staff—a bonus with the current staffing shortages and tight budgets. Separate solutions enable laboratories to choose those products that best match their needs. Ideal products will offer flexibility and the ability to tailor rules and workflows to maximize quality and efficiency.
And while the systems should be chosen for their individual value, it’s imperative to keep integratability in mind. If the systems do not work well together, their maximum value is lost, particularly if manual work-arounds are required. In addition, they need to work with other systems, such as the emergency medical record (EMR), as well.
“A billing system has the highest level of connectivity requirements of any software package that a laboratory uses and has to be integrated with just about everything,” says Lâle White, CEO, XIFIN Inc, San Diego.
Integration means a billing system can communicate with other databases to search for and find information that can ensure proper billing, testing, and compliance at both the front and back ends. Newer features on billing systems address areas where compliance or collection continues to be an issue.
Laboratories can now automate copay information to enable collection at time of service. Eligibility rules can help to prevent laboratory testing on specimens for which there is no reimbursement. Enhanced processes can ensure that tests are billed at result, rather than when ordered, a compliance issue for many laboratory information systems.
Some of the improvements stem from new capabilities; others are responses to a changing environment. Regulations, codes, and reimbursements are in continuous flux, and it can be a full-time job just to keep up with the changes. But fall behind, and the consequences can be severe: incomplete, improper, or nonpaid payments; noncompliance and the resulting penalties; and a waste of resources in a resource-conscious time.
FITTING THE BILL
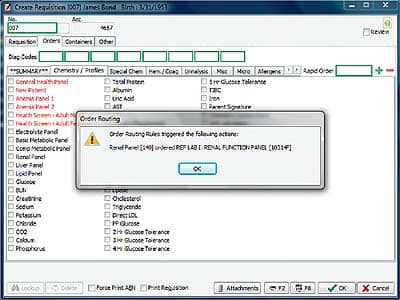
With CompuGroup Medical’s LabDAQ LIS, routing rules can be established so that, based on the patient’s insurance contract, if the test needs to go to a designated reference lab, it will be automatically routed.
While a laboratory needs to remain budget-conscious, the billing system is not necessarily a place to search for a bargain. Purchasing a system without paying attention to the needs or integration issues can actually waste money, not only that lost from a resulting inadequate billing process but also that spent on the mismatched product.
“It’s really important for the customer to know what they need that system to do for them,” says Dianna Powell, presales clinical consultant on the laboratory team, Merge Healthcare, Chicago. “The requirements of a physician’s office laboratory are going to be vastly different from the needs of a regional reference laboratory or those of a rural health facility.”
Complicating things further is that most laboratories are actually a hybrid. “Whereas laboratories might have been partitioned 20 years ago and focused on their own hospital inpatient work, it’s not that way anymore,” Powell says. “Every hospital has to offer outreach to the community and work as a reference laboratory as well—and the billing rules in those scenarios are different.”
Merge LIS gets around this with the ability to route charges based on different criteria, such as where the specimen was collected or the associated ordering physician. In some instances, the associated billing system will post charges to two separate systems.
White suggests one of the most logical ways for a billing system to deal with the complexity associated with billing is to use a rules-driven system with the lowest level of granularity. The system can then work easily with simple one-test orders to complex molecular diagnostics panels.
“You need the flexibility to have the building blocks at the lowest level, and then the system needs to have some flexibility in rules and consolidation to put those building blocks together in a manner that each payor wants to see,” White says. The entire process is automated and should require clerical intervention only infrequently.
SEPARATE CHECKS
This level of specificity is more likely to be found within a billing system than an LIS with a billing module or billing capabilities. “Even if the LIS can submit claims, it most likely is going to lack the advanced tools, such as claim scrubbing and revenue cycle management, found in practice management and billing software,” Laughlin says.
Some LISs do offer coding assistance. “Medical necessity checking can take place at the LIS to ensure that the appropriate diagnosis codes are provided for the procedures completed, and routing rules can be established so that, based on the patient’s insurance contract, if the test needs to go to a designated [reference] lab, you can run rules to automatically route the order to those labs,” Laughlin says.
However, many LIS billing modules are simpler, often just generating bills or focusing on one specific market type, such as a POL. “The logic is to find the LIS that fits your environment best, find the billing system that works for your environment best, and marry those two together very effectively,” Powell says.
CHECKING THE MATH
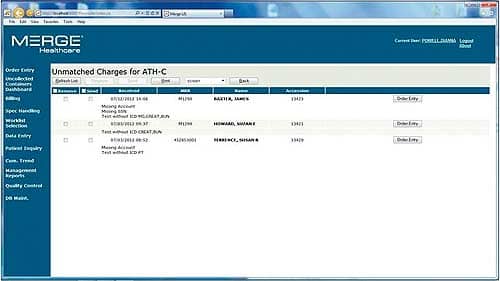
Merge LIS by Merge Healthcare uses a rules-based algorithm to route orders correctly and prevent the lab from billing—and performing—tests for which it will not be reimbursed.
For the marriage to be effective, the two systems must be compatible. “It’s really critical during that sales process to discuss the integration between the two systems,” Laughlin says, cautioning that some of the lower-end systems cannot handle billing interfaces.
If two vendors have not yet interfaced their products, the discussion about the potential should begin very early. “You want to make sure the integration can be completed without significant costs for customization,” Laughlin says.
Technically, use of the HL7 standard is supposed to make the process easy. In reality, however, “everyone has taken the standard, interpreted it in their own way, and put some things with it that are nonstandard, resulting in hundreds of standards being written for integrations with each different system,” Powell says.
The more differences between the specifications of two vendors, the more expensive the integration will be. Some companies have developed innovative solutions to reduce the need for extensive code rewrites. Merge uses scripted interfaces; XIFIN uses the Web.
“We designed our product as a Web-based system to allow two-way, real-time communication,” White says. “It does not require any hard proprietary interfaces or an interface engine but simply sends information to and takes back information from any of the products as a Web service.” This opens up infinite connection possibilities, and XIFIN offers more than 30 Web services that allow parallel file maintenance within any product residing in the laboratory.
“So it not only fully integrates the billing system with everything, but it also provides for those products a single point—using the billing system—at which they can get any of the data in any of their products,” White says.
CALCULATIONS AND COMPLIANCE
Better communication abilities translate to better system capabilities. The more information that can be shared and the more rules that can be written and followed, the more automation can handle the workflow with the resulting benefits. Greater accuracy in billing and coding can mean improved collections and reimbursement as well as additional advantages in regard to efficiency. “The billing department is another catch area where laboratories can correct the issues before they are transmitted,” Powell says. “It saves work and time.”
The workflow can be impacted as soon as the patient comes in. “We’ve developed a host of new products that will help our customers and which include Web services for front-end edits that go all the way to the EMR and physician’s desk, determining eligibility right at the point of draw,” White says.
Some LISs can handle this portion of the workflow. “We want to be able to look at the content of an order and know that using a rules-based algorithm within the LIS, the order will route accordingly so that the laboratory doesn’t inadvertently try to bill for something that it is never going to get reimbursed for,” Powell says.
Performing tests ineligible for reimbursement is one area where a lot of laboratories face a large amount of error and lost money. Another is upfront collections. “There is about 30% to 40% bad debt associated with upfront collection, so our customers are really making a concerted effort to collect as much of the copay and deductible at the time of service,” White says.
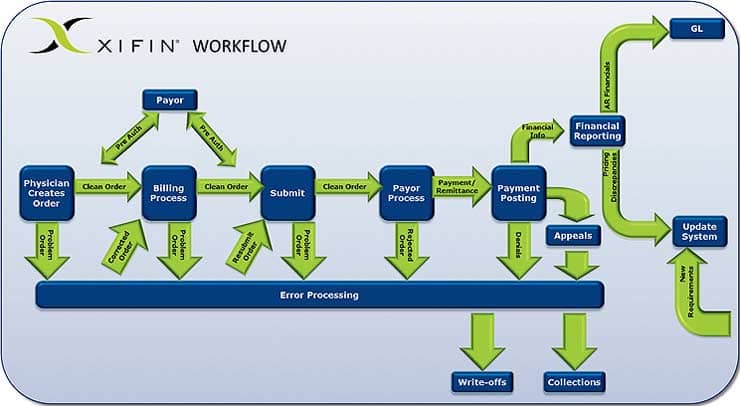
The XIFIN laboratory billing system automates a large part of the process with rules-driven workflow and comprehensive functionality that manages each step and transaction experienced by diagnostic labs and is designed to handle exceptions.
Eligibility rules can provide the level of insurance and copay but do not provide dollar amounts. Integration with a billing system that lists revenue at the exact amount to be paid can. “That allows the ability to provide the exact amount of insurance and copay to the laboratory at the time the patient is in front of them, so they can collect it,” White says. XIFIN also offers a patient payment Web service that the lab can use to accept payment by check, debit, or credit card, helping to further ensure collection.
On the back end, properly integrated systems can ensure compliant billing. Many LIS and EMR systems bill for a test when it is ordered, rather than when the result posts. “By the time you QNS [quantity not sufficient] the test, the charge has already been posted to the PM [practice management] system and billed to the insurance company, which is a fraudulent billing practice,” Powell says.
Correcting or mitigating this practice can create inefficient and time-consuming work-arounds. “So the billing system does want to get from the LIS system, for example, not just all the tests that were ordered but when they were final reported and what was final reported,” White says. This closes the compliance loop and allows a full reconciliation.
KEEPING UP WITH THE PAYORS
Of course, complicating matters further is the fact that codes and policies are constantly changing. “Even the largest labs with all the resources in the world find it a very, very difficult task [to keep up] because there’s no standard way of accumulating all of the data,” White says. “There are several vendors that sell pieces of it, but nowhere is there a complete, comprehensive list.”
XIFIN is able to offer its clients updates of this nature because it maintains an entire department dedicated to reviewing the electronic transmissions that come back from payors for anything new that has not been previously published or known.
“We maintain 100% of the published information—which includes multiple years of CPT codes, ICD-9 codes, payor edits, current coding initiative edits, OCE edits, all of the payor-specific edits—in one database across the board,” White says. Data entries into the system are crosschecked against the database and not accepted if they do not match current requirements.
The breadth of XIFIN’s referential information is unique, although many companies do offer some sort of update service. CompuGroup works with a third party to provide quarterly medical-necessity updates to LabDAQ customers. Merge also uses a third party to update all of the tables that have been imported into its system, such as CPT codes. Merge LIS clients can enroll in the subscription-model program to receive updates as they occur. XIFIN also uses a subscription-based model for its products, and despite the long-term investment, White suggests the system offers a return within the first 6 months.
Companies are now preparing for the upcoming switch from ICD-9 codes to ICD-10. The deadline has been postponed 1 year, from October 1, 2013, to October 1, 2014, but it is coming. Though it’s too early to begin preparation in earnest (“the codes are probably going to be updated,” Laughlin says), vendors should have a plan of action.
Part of the challenge will be ensuring that the interfaces between systems continue to function. The recent conversion to 5010 standards from 4010 for electronic health transactions exposed the difficulties in reformatting a claim submission. “Everyone, from the billing system to the clearinghouse to the insurance carriers, had to upgrade their systems and be ready, but it was a struggle, and laboratories and practices weren’t getting paid,” Laughlin says. The slow process is one reason administrators agreed to postpone the ICD-9/ICD-10 conversion.
Perhaps less difficult but no less complicated are the updates required to meet meaningful use standards. “Upcoming phases are going to address decision support regarding how and when a test is ordered,” White says.
The automation of these workflow processes helps to improve laboratory performance along with profit. “The more you automate a system and an interface, the more you’re able to handle, and your throughput can increase,” Powell says. “Whereas a billing department that lacks some of the automated features winds up dealing with a backlog and staff touches the same piece of paper multiple times as they go through the process of correcting, sending redeterminations, and rejustifying work that’s been performed weeks or months previous.”
For these groups, it doesn’t matter if the LIS came first. The addition of a billing solution will help to improve collections, ensure compliance, save time, increase efficiency, and grow volume—or more simply turn tests into revenue.
Renee Diiulio is a contributing writer for CLP. For more information, contact Editor Judy O’Rourke, .


