
Orchard Pathology system showing clinical and anatomic results and diagnosis all on the same report.
Lab outreach and electronic health record (EHR) management are undergoing revolutionary change. According to Curt Johnson, COO, Orchard Software, Carmel, Ind, change has come in the industry faster in the past 24 months than in the previous 5 years.
The reason? The American Reinvestment and Recovery Act and meaningful use regulations for laboratories. Such health reforms are affecting clinical labs by putting more focus on the importance of laboratory data, says Sandy Laughlin, LabDAQ product manager, Laboratory Solutions, CompuGroup Medical, Reisterstown, Md. And Johnson says governmental monetary incentives and disincentives have created a higher demand not only for smaller and medium-sized independent reference labs and hospitals to keep pace with the larger ones regarding EHR, but also in the move toward integration and consolidation of clinical and anatomic pathology and molecular functions in one diagnostic lab. This puts hospital labs doing outreach and the smaller independent labs at greater risk, since they’re being required to take on the integration capabilities of the larger labs.
Johnson says this higher demand was already occurring, but the governmental mandates greatly accelerated the process. Without that, the changes would have evolved less rapidly, he says, but they would have still taken place.
Smaller labs must now be not only capable of moving results to EHRs, but also be able to support the above-mentioned integration of functions. “It’s a challenge for them to retain their current business, and they are running the risk of losing clients,” he says.
The challenge is to provide electronic lab results in a structured and mineable format. But this can also be seen as an opportunity for some. Significant financial incentives can sweeten the pot for providers and hospitals to embrace the EHR in their facilities. However, for independent labs and hospitals doing outreach, there are no monies available to them for the integration of the client’s EHR, Johnson says. Without this integration, some providers and hospitals may feel the need to switch from one reference lab to another to meet meaningful use criteria for integration to qualify for incentives. This is another downside for the smaller independents.

The 4medica iEHR CPOE Module allows physicians to place all orders (such as ePrescribing, radiology, pathology, and laboratory orders) from a single viewable screen.
The other challenge that has evolved indirectly from the EHR requirements is the previously mentioned trend toward more integrated diagnostics and where clinical and anatomic pathology and molecular diagnostic results need to be electronically delivered to the EHR. However, this presents its own, more complicated set of difficulties, Johnson says.
“Most think of LIS data as quantifiable, structured, and easily transferred to an EHR. But anatomic pathology diagnosis has a history of being text and can also include images and diagrams,” Johnson says. “Molecular results also include many images and descriptions, which may make them difficult to integrate into the EHR. These issues are already taxing HL7 integration teams.” The challenge is to develop integration engines that can accomplish this consolidation.
However, he says Orchard’s challenge is to let the market know that it already has this capability in anatomic and molecular result delivery. The firm developed its current Orchard Pathology system to generate structured data, and it turns out that “now it’s what everyone wants,” Johnson says. It combines convergence and delivery of results in a structured format that is easily integrated.
THE NEXT CHALLENGE
Johnson says the next challenge is to go beyond the HL7 to HL7 model, to find a more efficient solution by creating one pipe to all EMRs; and that is already being accomplished through the use of such technologies as Web services and cloud computing, using one feed to connect to everything, thus streamlining the process, he says.
According to Laughlin, facilities that have implemented lab outreach programs work very closely with EMR vendors, as many providers require that the laboratory results be made available in the EHR software. Many laboratories are implementing outreach products for handling the multiple EHR interfaces as opposed to the LIS vendor. This interface service for facilities conducting outreach is moving away from the LIS vendor and to the outreach vendor.

The 4medica iEHR Patient Chart provides a unified view of all patient documents (such as inpatient, outpatient, and outreach) by facility type.
Each EMR vendor has its own methodology, she says, varying from vendor to vendor. HL7 2.0 is the baseline standard of communications.
One of the stage one meaningful use menu set objectives (facilities must implement five of the 10 menu set objectives) is to incorporate 40% of clinical lab tests’ results as structured data in the EHR. “It is anticipated that this will be a core menu set objective meaningful use criteria,” Laughlin says. “It is also proposed that LOINC (Logical Observation Identifiers Names and Codes) be implemented for identifying laboratory and clinical test results. The LOINC will be used when sending data from the laboratory to the EHR.” (LOINC applies universal code names and identifiers to medical terminology related to electronic health records to assist in the electronic exchange and gathering of such clinical results as laboratory tests, clinical observations, outcomes management, and research.)
Oleg Bess, MD, founder and CEO of 4medica, Culver City, Calif, agrees that physicians are increasingly adopting EHRs. For clinical laboratories slow to adopt the technology, EHRs offer an efficient, fast, easy-to-use way to transmit results to physicians. According to the Centers for Medicare and Medicaid Services (CMS), “The Medicare and Medicaid EHR Incentive Programs provide a financial incentive for the ‘meaningful use’ of certified EHR technology to achieve health and efficiency goals. By putting into action and meaningfully using an EHR system, providers will reap benefits beyond financial incentives—such as reduction in errors, availability of records and data, reminders and alerts, clinical decision support, and e-prescribing/refill automation.”
The strategy is working. And Bess also agrees that although labs are following suit slowly, their usage is expected to increase.
Bess leads 4medica’s business strategy, product development, and go-to-market initiatives across inpatient, ambulatory, and other care settings to meet demand for affordable and rapidly deployable cloud integrated electronic health record (iEHR) connectivity solutions. “Meaningful use has changed the landscape for labs as well,” he says. “For our lab customers, we see a wide range of labs from small to large, covering 10% to 20% of physicians already owning an EHR. This has grown from only about 3% to 5% of physicians just 3 years ago. Many use Quest Diagnostics, and some do not have full EHR systems. Smaller labs are less likely to have EHR solutions.”
But in the coming years, the 20% of physicians who use EHRs is expected to grow 80% to 90%. That percentage increase will be due to financial incentives and disincentives to their usage, Bess says.
And the market is bearing this out, he adds. Most physicians either are looking for EHR solutions or have made a decision to purchase. The current practice of labs using outreach lab solutions to provide physicians a few test results is unsustainable. “No doctor wants to view two computer screens to look up test results,” he says.
The lab must either interface with the physician’s EHR or offer a smooth transition to transfer data from outreach solutions to the physician’s system. “Labs are between a rock and a hard place; but at 4medica, we have certified solutions that are transparent and compatible with outreach solutions. We are well-known for creating interfaces for labs and physicians possessing EHRs,” he says.
“Our iEHR can be turned on instantly,” Bess says. “Everything is Web-based, and the system can be leased very inexpensively. We even offer a free version for support.” Activation is as simple as clicking a button, such as “patient’s chart,” on the navigation bar. Documents and charts can be viewed from there.
Bess wonders about vendors selling stand-alone outreach solutions. “They will have to expand,” he says. “And we will probably have to partner with another company to integrate all records—medications, test results, etc—for a comprehensive record.”
Though the lab industry has experienced significant change, the next decade will make all the difference in the way labs deliver results to physicians. “Printing results will become a relic,” he says. “Many more labs will be relying on EHRs, eliminating the need for outreach altogether.”
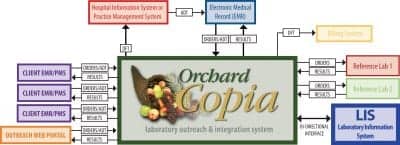
Integration diagram showing how the Copia Integration system helps to link the lab with its client provider EHRs.
ANOTHER ADVANTAGE OF EHR
The EHR offers another advantage that labs and physicians want: the ability to seamlessly move from one care setting to the next without investing in two different types of lab and e-medical records systems.
4medica offers a cloud-computing system for medical record storage. The firm was founded in late 1998, and by 2000 it had already developed a Web-based solution, considered extremely unique at the time, but which has since become widely accepted. “Today, our cloud solution is well-developed and features rich state-of-the-art technology,” Bess says.
The company is converting its database to the kind used by Google. There are more than 30,000 physicians who receive test, lab, and radiology results through its system. “Labs, although not legally bound by HITECH and meaningful use actions, nonetheless are directly affected because those regulations do impact their physician customers,” he says. The Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted as part of the American Recovery and Reinvestment Act of 2009 to encourage the adoption and meaningful use of health information technology.
Bess says the biggest industry buzz is the Accountable Care Organization (ACO), which creates a care structure in which physicians, technicians, and consultants all share in the making of a single payment. This Kaiser-like system is a radical shift for many facilities, he notes.
According to CMS, an ACO is “an organization of health care providers that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional fee-for-service program who are assigned to it.”
Bess says labs, hospitals, and physicians’ offices must closely integrate. “It’s not surprising that Kaiser was a pioneer in implementing health care technology,” he says. “Integration will be challenging, but labs that seize the opportunity will benefit in the long run. To financially survive, labs must learn how to support not only their doctors’ EHRs, but also hospitals’ EHRs.”
The 4medica system is certified for both inpatient and outpatient environments. “We recognize the need for deep integration of data,” Bess says. “Our system will enable both labs and hospitals to seamlessly share and talk to major labs and emergency rooms.”
Gary Tufel is a contributing writer for CLP.



