Molecular diagnostics are replacing culture as the gold standard for the diagnosis of respiratory viruses but continue to share the stage with conventional methods that offer advantages of speed and convenience.
The “science” of alchemy has not yet been able to modify molecules to obtain gold, but in the field of respiratory viral diagnostics, science has achieved gold by manipulating molecules. Many suggest that molecular diagnostic methodologies have replaced culture as the gold standard for the detection and differentiation of this group of diseases.
“I think there’s a shift taking place, even at the FDA level, where culture used to be considered the gold standard method. There are now plenty of publications out there that show it may not be the most sensitive, specific assay, and molecular is taking the place of the gold standard,” says Steven Visuri, PhD, director of research and development for Prodesse Products, San Diego.
However, even though molecular diagnostics offer greater accuracy, they do have some limitations that culture, direct fluorescent antibody (DFA), and rapid immunoassay tests overcome, assuring these conventional methods will continue to be used, at least in the short term. In selecting which diagnostic to use in the evaluation of respiratory disease, clinicians and laboratorians must balance many needs, including clinical value, accuracy, efficiency, expense, and ease of use.
Value in Value
The primary factor all laboratories are concerned with is clinical value. Producing a test result quickly or easily means nothing if that result offers neither clinically actionable information nor any medically useful data.
“The results that are the most valuable to clinicians are the ones that drive immediate medical decisions. Should I treat with Tamiflu [oseltamivir phosphate] or not? Should I treat with an RSV medication if I have a virus or not? Should I treat with erythromycin or not for bacterial infections?” says David H. Persing, MD, PhD, executive vice president, chief medical and technology officer of Cepheid, Sunnyvale, Calif.
Secondary information from respiratory viral panels provides less direct but still medically useful data. “The ancillary information that comes from the test results has value but at a lower level than that provided from the results that represent actionable treatment. If the patient has parainfluenza virus, there is no available therapy, but at least the clinician knows the patient has a virus and can tell the concerned parent that the patient has a virus, doesn’t have a bacterium, and doesn’t need antibiotics. So it is indirectly useful from that standpoint,” Persing says.
Paramount to usability is reliability. “When you get things like the H1N1 pandemic, it becomes important to have a test, first, that you can rely on and, second, that helps differentiate what you’re in fact dealing with because there are real consequences as to how you deal with those patients,” says Eric Tardif, senior vice president of corporate strategy with Gen-Probe Inc in San Diego.
Sensitivity and Specificity
Prodesse’s ProFlu-Plus is a real-time multiplex RT-PCR kit for the detection and differentiation of influenza A, influenza B, and RSV with results delivered in less than 4 hours.
Respiratory viruses, particularly influenza, present a special challenge in their detection because of their natural tendency to evolve quickly. “Many of the respiratory viruses, with the exception of adenoviruses and a few others, are RNA viruses. RNA viruses mutate more rapidly than DNA viruses, and in the case of influenza, it’s an ever-changing target. So it’s difficult to pin down these viruses within a snapshot of time relative to their evolution,” Persing says.
Molecular diagnostics have the advantage in detection because they can target relatively stable areas of a virus, therefore bypassing some of the more easily mutated sequences of its genetic material. “With molecular approaches, you can analyze the DNA sequences or RNA sequences by different strains and identify the regions which remain consistent over time,” says Jeremy Bridge-Cook, PhD, senior vice president of the Assay Group at Luminex Corp in Austin, Tex.
The company’s inclusion of the matrix gene, a general flu detection site, in its xTAG Respiratory Viral Panel enabled the diagnostic to identify H1N1 as a new strain. “That still leaves the question about whether or not we want to put a new probe for H1N1 in the product and get that cleared,” Bridge-Cook says.
It’s a question rapid test manufacturers must constantly grapple with. “The outside of that virus is continually changing. However, the nucleoprotein on the inside has minimal evolutionary pressure on it to change,” says Norman Moore, PhD, director of medical affairs for Alere Inc (formerly Inverness Medical Innovations Inc), Waltham, Mass. Rapid assays, therefore, target the nuclear protein (using antibodies) of a specific virus.
As viral patterns change every season, so does the performance of rapid tests. “It’s not the tests bouncing up and down in performance—all rapid tests are doing analytically about the same year to year—it’s new viral strains that have different characteristics,” Moore says.
These strains may come and go, leaving companies wondering whether they should invest in adding a new one to their menu during times of pandemic, such as H1N1. “The FDA requires us to have a clinical trial to make a significant change to a product. And so, because the clinical trial would take a season and then several months after that to actually submit and receive a response back, by the time you’ve had a trial on a particular virus to get clinical performance, that strain may be gone,” Moore says.
Speed and Convenience
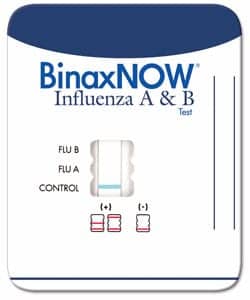
Alere AB combo card.
Rapid tests, therefore, do not provide the greatest sensitivity and specificity among respiratory viral diagnostics, but they are able to provide clinically useful information in a very short amount of time—often
15 minutes or less. “For influenza, you have to give the antiviral [medication] within the first 48 hours of symptoms to have the best efficacy. Coincidentally, the rapid tests have their best sensitivity in those first 48 hours as well since the viral titer is highest early in infection,” Moore says.
An early diagnosis for influenza could then lead to treatment resulting in lessening the physical symptoms for the patient and less contagion. “When you start to feel that first ache, that’s when you’re putting out the most virus. Because the virus wants to get passed around, it wants to have its highest titer when you’re able to be walking around instead of thinking, ‘I’m feeling kind of ill,’ ” Moore says. Late in the infection, a person may feel worse but will probably be excreting less virus, and so the rapids will not perform as well.
Generally, clinicians will use a rapid immunoassay early, often during triage at the point of care. Positive results from a rapid test are generally considered reliable. Physicians can prescribe treatment, if available, on the spot. “If the patient presents with clinical symptoms, and you perform a lateral flow test and it’s positive, then it helps confirm the clinical diagnosis, so there still remains and always will remain utility for the standard lateral flow point-of-care test,” says Carl Stubbings, vice president of sales and marketing for Focus Diagnostics Inc, Cypress, Calif.
Questions arise, however, when the result of a rapid diagnostic is negative; confirmatory testing is often required. The negative result could be related to a host of factors, from poor sample collection to a new strain of virus that produces a lower titer. Moore suggests that improper sample collection played a significant role in the poor performance of rapid immunoassays during the H1N1 pandemic.
“We saw a lot of people collecting samples that weren’t used to taking clinical samples, and quite often, they were doing it poorly. If you can’t get a good sample, you can never overcome that with a rapid diagnostic,” Moore says. Nasopharyngeal swabs and nasal washes are reported to have better performance than nasal swabs but are more intimidating for the patient. Moore points to the web site of the Centers for Disease Control and Prevention for educational materials to share with physician offices, satellite labs, and other outside facilities.
Expense and Ease of Use

The Integrated Cycler is a realtime PCR instrument with a footprint of less than 1 square foot.
Rapid tests themselves in general, though, are easy to use, typically regulated under the CLIA [Clinical Laboratory Improvement Amendments] waiver. They can be performed at the point of care by personnel with proper training, including technologists, nurses, and physicians. Molecular tests, by contrast, require specially trained technologists and special equipment to run. The associated cost and limitations of the “new gold standard” are driving manufacturers of molecular diagnostic systems to focus on ease of use as they develop next-generation technologies.
“We’re seeing more and more laboratories make the decision to adopt more expensive but easier-to-use technology because they don’t have available the highly trained staff to run the tests that most DNA diagnostic testing requires,” Persing says. He cites a number of companies developing moderate-complexity molecular technologies in addition to Cepheid’s efforts.
In-house, easy-to-use systems will provide the facility with advantages related to turnaround time, workload, and revenue. “It’s important for companies to be out there with something that is current and ready for customers to be able to use so they don’t have their only reliance on public health labs,” says Prodesse’s Karen Harrington, PhD, clinical affairs and clinical lab manager, as she recalls the overload and turnaround delays experienced by public health laboratories during the H1N1 pandemic.
Equipment investment is often returned through improved patient care and outcomes along with decreased medical costs for that care. In-house ownership provides in-house control, meaning that specimens can be handled as the laboratory sees fit—ie, batching versus single sample runs. In the past, batching has meant greater efficiency, both time- and cost-wise, but as process improvement methods take hold, laboratories are approaching workflow differently and more seamlessly.
In streamlined operations (and with the right technologies), samples can be dealt with on a one-off or “stat” basis. “I think a patient coming into the emergency room with a respiratory infection who is going to be admitted to the hospital is an emergency because they need to know what the patient has. Admitting a patient who’s positive for influenza into a hospital setting without isolation is very problematic because in that setting, those infections can spread both to medical staff and other patients and very readily cause a major problem,” Persing says.
Usability
Ideally, clinicians want answers and want them fast. One certain way to speed turnaround is to run tests simultaneously. “Individual tests create a heavy workload for the clinician and laboratorian. If we can cover many respiratory viruses with one test, the laboratory doesn’t have to worry about the workload sample volume or sample numbers. The cost is then very low, similar to a single viral test, and they’re easy. So nowadays people are looking for how many pathogens we can cover with one test and how quickly,” says Jong Yoon Chun, PhD, CEO of Seegene Inc, with US headquarters in Rockville, Md.
Although rapid antigen tests may be designed to detect more than one type of test, they are typically limited in their ability to multiplex. Molecular approaches find it much easier. “One of the greatest advantages to PCR technology is the fact that it doesn’t care whether the nucleic acid came from a virus, a bacterium, a parasite, or a blood cell—it’s all DNA or RNA to PCR. And one can put together panels of 15, 20, 30 targets and still get good sensitivity levels for the detection of each one of those individual targets,” Persing says.
A test that can provide information on all types of respiratory disease, whether viral, bacterial, or other, would be incredibly useful for the clinician. A test that could do this in a short time frame at any time of day would be ideal. “What laboratories are looking for is something that can provide the accuracy of PCR but with the turnaround time more like one of the rapid tests. In other words, they’re asking for the best of all worlds, and I think they will ultimately get that with the way the technology is evolving,” Persing says.

To track developments in respiratory testing, watch www.clpmag.com.
Many industry watchers agree that molecular approaches are the primary method for respiratory viral diagnostics in the future, and are the gold standard method for the present. “We see a series of markets being served by mature technologies that will convert over time to molecular, with the need particularly acute in areas where current methods are unreliable, the workflow is poor, or the clinical decision is at a level where you need confidence in the result in a way you can’t get from other methods,” Tardif says.
So the biggest question in the field of respiratory viruses is not how do we detect and differentiate these diseases. “In the 20-odd years I’ve been in this industry, there has always been another virus that’s caused another problem, so I guess my question is what do I think the next one is going to be?” Stubbings asks. Only time and science will tell.
Renee Diiulio is a contributing writer for CLP.