Color, San Francisco, has received FDA emergency use authorization (EUA) to offer covid-19 testing without clinical monitoring. The Color test now supports unmonitored testing both at-home as well as onsite for congregate settings, and it is unique in the United States because it is designed for large population and public health initiatives rather than consumer-initiated testing. This update to Color’s testing process is part of the company’s strategy to further increase access to covid-19 testing by addressing technical, supply chain, and logistical bottlenecks in the testing process.
“Covid-19 testing access is difficult because it is not a single problem—it’s an array of distinct, but connected, problems. The country needs a set of holistic solutions that solve each part of the chain of testing bottlenecks, and that is what we strive for at Color,” says Color CEO Othman Laraki. “This EUA enables us to dramatically increase the availability and accessibility of testing in high-risk, high-exposure contexts, which we believe is essential to supporting a safe re-opening of our society.”
Color’s strategy has centered on designing an integrated solution to address bottlenecks across the entire testing lifecycle. This EUA is an amendment to Color’s original filing, which granted the company authorization to use a loop-mediated isothermal amplification (LAMP) process in a centralized laboratory for covid-19 testing. LAMP is a method of amplifying segments of viral genome within covid-19 test samples to detect the presence of the virus. LAMP molecular testing technology delivers covid-19 test results with accuracy equivalent to the current gold standard method, reverse transcription polymerase chain reaction (RT-PCR), but lends itself more readily to high-throughput automation and rapid lab scaleup.
Color’s original EUA was designed to address supply chain and turnaround time limitations. Today, Color supplies the majority of the testing for the city of San Francisco and other major public health test initiatives, with an average 24-hour turnaround time for test results.
This latest EUA amendment makes important advances in addressing two key bottlenecks that still limit access to testing: the lack of sufficient clinical staffing to collect samples and the shortage of sample collection kits.
First, Color’s covid-19 unmonitored testing kit is permitted for use without direct clinical monitoring. This relieves an important bottleneck in the testing process by reducing the number of healthcare workers involved. The process authorized by the FDA makes it possible for patients to utilize Color’s test at home and return a sample by mail, as well as on-site as part of a test collection process. The latter makes it possible for Color’s test to be used to support onsite testing in critical public health contexts, such as community testing sites, places of employment, universities, and more. Supporting broader testing access in these contexts is vital to reducing the high risk of disease transmission and exposure.
Second, Color’s unmonitored test kit makes use of a dry nasal swab. Other unmonitored covid-19 testing options either require higher-cost saliva samples or nasal samples with a stabilizing solution such as saline. Color’s decision to utilize a dry nasal swab uniquely addresses a number of limitations. The dry nasal swab format consists of a spun polyester swab and tube — both of which are in abundant supply. Moreover, the lack of viral transport media in the tube (saline or other stabilizing solution) resolves usability issues, like spillage and safety, which necessitate more careful handling and complex kit design. Color has also found that dry nasal swabs provide a more consistent sensitivity and stability profile, representing a favorable set of tradeoffs for unmonitored collection and mail-based handling.
“Every day, our scientists are working on new ways to optimize testing for population health,” says Alicia Zhou, chief science 0fficer at Color. “The EUA to use dry swabs for unmonitored testing sets Color up to continue to scale the capacity at our lab, provide relief to healthcare workers who are spending valuable time collecting samples, and expand access to fast, accurate testing for high-risk populations, essential workforces and people in our communities.”
For more information, visit Color.
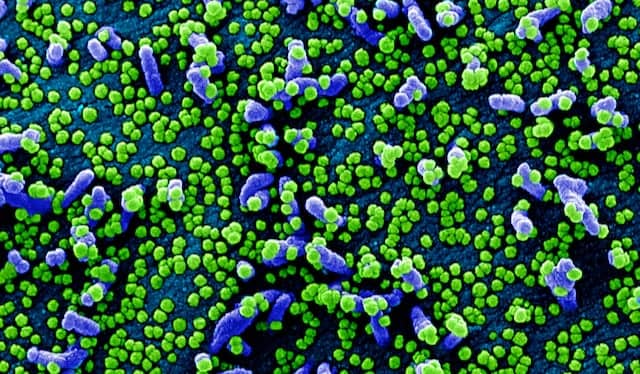
Featured image: Colorized scanning electron micrograph of a VERO E6 cell (blue) heavily infected with SARS-COV-2 virus particles (green), isolated from a patient sample. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID.