A smart bandage consisting of a wearable sensor that can conduct real-time, wireless, point-of-care assessment of chronic wounds has been developed by a research team led by Lim Chwee Teck, PhD, a professor from the National University of Singapore (NUS) Department of Biomedical Engineering and Institute for Health Innovation and Technology (iHealthtech), in collaboration with clinical partners from Singapore General Hospital.
The novel sensor technology of the smart bandage can detect temperature, pH, bacteria type, and inflammatory factors specific to chronic wounds within 15 minutes, which enables fast and accurate wound assessment. The research was first published in Science Advances.
With a rapidly aging population, healthcare providers are seeing more patients suffering from non-healing wounds such as diabetic foot and chronic venous leg ulcers. About 2% of the world’s population suffers from chronic wounds, and the healing process is often interrupted due to infection or repeated trauma, leading to severe stress, pain, and discomfort to afflicted patients. For patients with diabetic foot ulcers, this can lead to more severe outcomes such as foot amputation.
Timely care and proper treatment of chronic wounds are needed to speed up wound recovery. However, this requires multiple clinical visits for lengthy wound assessment and treatment, which adds to the healthcare cost. According to the NUS team, their smart bandage innovation can help mitigate these consequences and relieve patients with chronic wounds from unnecessary distress.
Smart Bandage Promotes Personal Healthcare
Current clinical assessments of wounds rely on visual inspection, or collecting and sending wound fluid to a centralized laboratory to detect and analyze specific biomarkers. The whole process usually takes about one to two days and may impede proper, timely, and precise medical interventions. Although there are recent developments in flexible sensors designed for wound care, they can probe only a limited set of markers such as acidity, temperature, oxygen, uric acid, and impedance to diagnose wound inflammation.
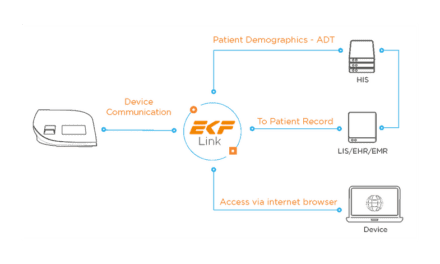
In response to these current limitations, the NUS researchers developed VeCare, a point-of-care wound assessment platform consisting of a wound sensing bandage, an electronic chip, and a mobile app. The bandage comprises a wound contact layer, a breathable outer barrier, a microfluidic wound fluid collector, and a flexible immunosensor.
According to the team, VeCare is the first wound assessment platform that can detect bacteria type and probe inflammatory factors, in addition to measuring acidity and temperature, within a single 15-minute test. The immunosensing bandage enables rapid assessment of wound microenvironment, inflammation, and infection state by detecting multiple chronic wound-specific biomarkers from wound fluid using an electrochemical system.
The microfluidic wound fluid collector attached to the sensor directs and boosts wound fluid delivery to the sensor by up to 180%. The design ensures reliable sensing performance regardless of the ulcer shape or size.
In addition, a chip integrated with flexible electronics is connected to the sensor to transmit data wirelessly to an app for convenient, real-time wound assessment and analysis onsite. The chip component, powered with a rechargeable battery, can be reused for subsequent applications.
The VeCare platform and mobile app enable physicians to monitor the condition of patients’ chronic wounds remotely, reducing the hassle for patients to travel to a clinic. The bandage complements the patient’s existing medical treatment while facilitating timely medical intervention for wound healing processes.
“Point-of-care devices coupled with telehealth or digital health capability can play a significant role in transforming the healthcare industry and our society, which is catalyzed by the COVID-19 pandemic requirements for safe distancing,” says Lim, who is Director of iHealthtech at NUS. “Our smart bandage technology is the first of its kind designed for chronic wound management to give patients the freedom to perform the test and monitor their wound conditions at home.”
Using Smart Sensors for Better Clinical Management
In collaboration with the Singapore General Hospital, a small clinical test of VeCare was conducted on patients with chronic venous leg ulcers. They successfully demonstrated that the platform is effective in the assessment of chronic wounds and enables monitoring of the wound healing progress with timely medical intervention.
“The VeCare platform is easily scalable and customizable to accommodate different panels of biomarkers to monitor various types of wounds,” Lim says. “The aim is to have an effective and easy to use diagnostic and prognostic tool for precise and data-driven clinical management of patients.”
The research team plans to further develop VeCare to meet safety, regulatory, and mass production considerations. The team will explore the incorporation of other appropriate biomarkers suitable for other wound types and use data in existing clinical workflows to improve diagnosis and treatment. The team hopes to test the technology on a larger prospective randomized clinical trial with different types of nonhealing chronic ulcers, such as diabetic foot and pressure ulcers.
Featured Image: The VeCare platform comprises (clockwise from bottom left) a chip, a wound sensor, a bandage, and an app for real-time, point-of-care chronic wound monitoring. Photo: National University of Singapore