As the primary health care decision-makers for families from cradle to grave in American society, women are attuned to health concerns throughout their lives as well as those of their families. Technological advancements in medicine work to combat disease and forestall the effects of aging, while at the same time, we are developing our understanding of the importance of healthier living, disease prevention and earlier interventions at every stage of life. The effective management of disease, if illness does strike, relies on careful monitoring of therapies made possible by advanced diagnostic techniques.
Osteoporosis is a chronic, debilitating condition, and 80 percent of its sufferers are women. We think of osteoporosis as a disease of old age, but the prevention of osteoporosis is a lifelong concern. By the time a woman turns 18, she has acquired 60 percent of her final bone mass, which ultimately peaks as she enters her 30s. In reality, osteoporosis can strike at any age. It is responsible for more than 1.5 million fractures each year, including 300,000 hip fractures, 700,000 vertebral fractures, 250,000 wrist fractures, and more. Half of women over the age of 50 have a fracture related to osteoporosis during their lifetime, and nearly one-fourth of those over 50 who fracture a hip die within a year of the incident. Modern diagnostic techniques and treatments such as Hormone Replacement Therapy and bisphosphonates can help to provide more effective management of this disease.
But even though our science is better and medical interventions have advanced, we may be stepping backwards in terms of preventing this disease during the crucial early stages of life, when both bone mass and habits are formed. Laurie Robinson, regional coordinator, Office on Women’s Health, Region I, United States Department of Health and Human Services notes, “Soda is now often the normative beverage for kids, and that is a societal change. Milk and soy milk, and beverages with the nutrition needed to build bones, have been replaced for many children with empty calorie drinks. The fact that we have non-nutritious snack foods and soda sold in vending machines in our school systems affects kids’ eating patterns and meal choices. At the same time, we have cut back on physical education classes and reduced opportunities for exercise. Many children live in neighborhoods where it’s not safe to play outside, and as we’ve lost those environments, we’ve lost opportunities for kids to develop bone strength through exercise and play.”
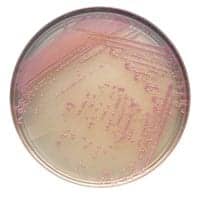
Another growing health concern linked to social change is the rise of infertility, due in part to the desire and ability to delay childbearing until an age when it is harder for couples to conceive naturally. While not considered a life-threatening condition, infertility can be a cause of terrible anguish for people with the instinct and expectation to experience family life with their own children. Here again, prevention measures and improved diagnostics hold the keys to better outcomes. The cause of infertility for approximately one in four couples who can’t conceive can be traced to a sexually transmitted disease, and untreated chlamydia or gonorrhea goes on to become responsible for 15 percent of female infertility. These conditions are both preventable and subject to benefit from early diagnostics. Highly sensitive diagnostic tests are also critical to treating infertility from hormonal causes, as those assays enable close monitoring of individualized therapies to aid in conception.
One of the amazing stories in medical science is the virtual eradication of hemolytic disease of the fetus and newborn (HDF/N). Once a devastating disease, HDF/N affected fetuses of Rh negative women and either caused fetal death or affected neonates with heart disease, mental retardation or severe anemia that required exchange transfusions. With blood typing tests, and treatments that have now become routine in the U.S., the past 30 years have seen the virtual elimination of the serious problems associated with infants of Rh-negative women. Among proponents of preventive health services, good prenatal care is widely accepted as the prime example of cost-effectiveness, and Rh testing and treatment is part of that standard.
One of the most frightening of diagnoses for a woman to receive at any time in her life is that of ovarian cancer. Although the incidence of this disease is comparatively low, it is known to be the most deadly cancer of the female reproductive system. With early diagnosis, however, survival rates increase dramatically. Early ovarian cancer is difficult to detect with physical examination, so in vitro diagnostics could prove critical for improved survival. While a true screening test may be some time off, tumor markers now available can aid in both evaluation of a suspected mass and management of known disease.
Ovarian cancer is not just a diagnosis of the childbearing years. Indeed, it is most common in women over age 60. All told, women today will live over one-third of their lives post-menopause, and while many women may believe that menopause signals the end of the need for a regular gynecological exam, the risk for reproductive system cancers actually increases with age.
Just knowing about health issues, however, is not enough. Robinson of the Office of Women’s Health explains that women often view their own health in relation to other things they are managing in their lives, including the demands of job, children, partner, and sometimes aging parents of their own. While women actively engage in health care through these roles, they may not be focusing enough on themselves. “Women often experience or think about their own health issues after they think about their other commitments or responsibilities,” says Robinson. “Though a woman may know about health screenings she needs (such as a mammogram, PAP or colorectal screening), she may put herself last, trying to juggle a lot of responsibilities. Even as we’ve made progress for men and women in the workforce, women still tend to shoulder the larger proportion of household and family maintenance activities, and that means they have less time for focusing on their own health issues.”
Insurance is also a major concern, both for women and for providers. Robinson points out that having health benefits that allow for prevention and screening, rather than just treatment, is critical. Moreover, the number of women who lack insurance coverage of any kind is greater now than ever, with nearly one in five women under the age of 65 uninsured in 1998. Eighty percent of these uninsured women are either in the workforce or married to someone who is. Low- and moderate-income women, women of color, and women with health problems are disproportionately represented among those without insurance. For all women, lack of insurance sharply compromises the ability to obtain quality healthcare.
In the face of financial and time pressures, information alone may not be enough, but it is still our greatest asset. “Women, and all people actually, need to have a good source of health information,” says Robinson. “They need to know that they are going to be a partner with their healthcare provider in managing their health.”
“Women are bellwethers for the health of the whole society,” she adds. Given the important role women play, from their influence over developing their children’s and spouses’ health habits, to providing ongoing care to the older generation, our society would do well to insure that women maintain their own health status. Offering support in the form of information, encouragement and research into diagnostic and treatment options that impact women’s health provide initial steps to success.

Osteoporosis is a stealth disease that catches thousands if not millions of women unaware. Debbie Reynolds believed the active dancing career that made her the darling of a generation had also developed her bones to the point where they would be able to withstand the destructive nature of this disease. That was before she received the diagnosis that her own bones were thinning, and she became celebrity spokeswoman for the National Osteoporosis Foundation (NOF).
Now the next generation – the baby boomers – is reaching the critical age for onset of this debilitating condition. The NOF estimates the number of women and men aged 50 and older who exhibit either low bone mass or osteoporosis at 44 million. To further compound the issue, NOF expects that by the year 2020, that number will expand to an estimated 61 million unless a great deal more attention is paid to this crippling, even life threatening disease. Take one 85 year old, add a hip fracture, and complications may lead to death. Spinal or vertebral fractures, another hallmark of the disease, can yield loss of height, severe back pain, and other disabilities.
Prevention holds the key to successful management of this health risk. Proper diet that includes calcium rich foods, regular weight bearing exercise, and avoidance of smoking and excessive alcohol are some of the simple steps anyone can take. Women must be especially watchful, as they are four times more likely than men to develop this disease, particularly as they lose the protective effects of estrogen in later stages of the life cycle. Osteoporosis is most prevalent in post-menopausal women, so attention to bone health, begun in childhood, gains importance again at the perimenopausal stage of life. Awareness of osteoporosis prevention, and knowledge about diagnosis and treatment, dramatically affect eventual health outcomes.
Normal Biologic Processes Cause the Problem
Laurence M. Demers, Ph.D., distinguished professor of pathology and medicine, Pennsylvania State University College of Medicine at the Milton S. Hershey Medical Center (Hershey, Pa.) explains that most bone mass is accrued between the ages of ten and 21. When optimal bone density is not attained, a person becomes a candidate for eventual fractures related to osteoporosis.
Although bone appears to be a rigid and unchanging structure, in reality it is in a constant state of change. The human body is always turning over new bone cells, with 10-30 percent of the adult skeleton remodeled every year through a process that includes two steps: resorption that removes bone cells and bone formation that places new cells into the bone structure. Bone mass is lower in women than men at all stages of life, so with less bone to lose, women are always at greater risk of becoming osteoporotic. When the rate of bone resorption and formation are equal, however, no loss of bone occurs. But in both men and women over the age of 30, resorption begins to outpace the rate of formation, and a net loss of bone results. That loss becomes precipitous in women following menopause, with the majority of female bone loss occurring five to seven years after menopausal onset.

In addition to diet and lifestyle interventions, there are available prescription treatment options for osteoporosis. Hormone Replacement Therapy (HRT) reduces the level of bone loss that accompanies hormonal changes. And in patients for whom osteoporosis has been diagnosed, prescription use of oral bisphosphonates can be used to slow the rate of resorption and in some instances to effectively build bone structure at the formation level. There are potential problems in the clinical management of patients prescribed medication for osteoporosis: some experience difficulties with malabsorption of medication, some may require a higher dose than originally established, and some may discontinue their medications due to unpleasant side effects.
A bone mineral density (BMD) imaging test measures bone density at the spine, hip and/or wrist and serves as the definitive diagnostic test to reveal the presence of osteopenia (early stage of bone loss) and osteoporosis as well as to predict the risk of fracture. BMD is capable of measuring changes in bone mass at time intervals of 12 to 24 months. Fortunately, there is a complementary technology that permits more frequent assessment of the effects of therapy.
Clinical Diagnostic Test Aids Evaluation
Cross-linked N-Telopeptides (NTx) provides a quantitative measure of bone resorption from urine samples. This clinical laboratory biochemical measurement can inform a physician when borderline bone loss is detected on BMD, and serves as a valuable adjunctive technique to evaluating a patient’s response to therapy.
Demers explains that the NTx assay values can provide the physician with information at three month intervals to determine if a patient is responding appropriately to treatment, which would predict a positive BMD result in a year. The NTx bone marker can be run on the Ortho-Clinical Diagnostics Vitros ECi Immunodiagnostic System using urine specimens. With either HRT or the use of bisphosphonates, these laboratory values serve as a powerful adjunct to the management of patients with early stage or fully developed osteoporosis.
Marla Ahlgrimm, R.Ph., CEO and founder of Women’s Health America in Madison, Wis., explains the approach her facility began twenty years ago with regard to HRT. As their patient population aged, WHA adapted its capabilities to address the needs of women with bone loss secondary to the hormonal shifts of menopause. “To enable practitioners to decide where to start treatment, we developed a program to help them determine which hormones were appropriate and at what dose ranges,” explains Ahlgrimm. Because physicians requested quantitative outcomes measures, WHA moved to using the Vitros ECi system to streamline reports about bone health for patients being treated with HRT. Ahlgrimm describes the NTx assay as a highly sensitive and specific marker for bone breakdown that enables more accurate treatment management. After a baseline value is determined, intervention is initiated. That could involve weight bearing exercise and calcium, but might also include HRT or other pharmaceutical products. Follow-up NTx studies are done in 60 to 90 days, and the physician receives a result to help guide the next steps. If the current regimen seems to be adequate, it will be continued until the next BMD.
The mission of Women’s Health America is to provide customized therapy for each individual patient, and Ahlgrimm reports that the use of urine markers to inform treatment decisions, “…has revolutionized HRT as it is practiced today.”
Osteoporosis Requires Timely Accurate Management
While Bone Mineral Densitometry provides the foundation for a diagnosis of osteoporosis, follow up care and monitoring of treatment relies on information from clinical laboratory tests that reveal the rate of bone loss with a urine biomarker. N-telopeptides offer frequent assessment opportunities in managing this disease.

For centuries, Rhesus disease, also called Hemolytic Disease of the Fetus/Newborn (HDF/N), puzzled medical science and harmed babies by the millions. But in the last three decades, better prenatal care and treatment advances have combined to virtually eliminate HDF/N in most countries.
One of the most respected international authorities on the disease, Dr. Kenneth Moise, Jr., says prevention of HDF/N ranks with the birth control pill as the most significant advance in women’s health care in a generation.
In 1968, there were 45 cases of HDF/N for every 10,000 live births. More than thirty years later, HDF/N has been reduced to between 6 and 10 cases per 10,000 live births due to the use of Rh immune globulin (RhIG) products like RhoGAM, developed by Ortho-Clinical Diagnostics. Pioneering work led by Ortho scientists in the 1960s set the dosing standard and treatment regime.
What once caused health problems in newborns such as anemia, jaundice, heart disease, cerebral palsy and in some cases fetal death is now remedied by administering two simple injections of Rh immune globulin in pregnant mothers whose Rh factor is different from that of their newborn child.
Blood Cell Incompatibility
Beyond the typing of blood as A, B, AB or O, a mother is at risk when she is Rh-negative and her baby is Rh-positive. Simply stated, the Rh-negative mother is missing a vital gene that provides a protein called the “D” antigen on the surface of her red blood cells.
During the birthing process, the unborn child’s blood cells can pass into the mother’s bloodstream where they are recognized as different than the mother’s. The mother’s immune system then begins a natural rejection process by producing antibodies to fight off the foreign Rh- or D-positive red cells. This process is called red cell alloimmunization.
Alloimmunization typically occurs after the delivery of a baby at the end of a pregnancy. But it can also result from other pregnancy-related events, such as abdominal trauma, induced termination of pregnancy or spontaneous miscarriage.
Rarely is alloimmunization dangerous during first pregnancies. That’s because a mother’s antibodies are weak and few in number. Subsequent pregnancies will likely exhibit more severe results as more potent antibodies attack and lower a baby’s red blood cell count. The result is HDF/N.
The Demographics of Risk
So who is missing this gene? Estimates indicate at most about 15 percent of the U.S. population is Rh-negative. Caucasians are most likely to lack the “D” antigen (15%); African-Americans (8%) and Asians (1%) face dramatically reduced dangers. Being Rh-negative presents no special health problems except when a person is giving or receiving blood and during pregnancy.
Basic medical tests reveal the presence of antibodies. The initial prenatal exam is usually the most comprehensive a woman will undergo. Routine blood workups reveal Rh status and could show whether any Rh antibodies are present. Doctors can determine a baby’s Rh status using amniocentesis.
Typically, Rh-negative mothers-to-be are given an RhIG injection around the 28th week of pregnancy, then another within 72 hours of birth if the newborn is Rh-positive. RhIG is given as a full dose injection for full term pregnancies or miscarriages that occur after the first trimester. RhIG treatments are also used when contact with fetal blood could occur during other events of a pregnancy. These would include chorionic villus sampling (CVS), amniocentesis, an ectopic pregnancy and vaginal bleeding. Where a mother’s Rh antibody level is extremely high, treatment could include an intrauterine transfusion of red blood cells through the umbilical cord. Thorough prenatal testing and treatment have combined to minimize Rh disease in newborns.

Dr. Kenneth Moise, Jr. is director of the division of maternal-fetal medicine at the UNC-Chapel Hill School of Medicine. He said the origin of the Rh-negative condition in America has been the subject of much speculation. “We didn’t know where it came from,” Dr. Moise said. “But something happened in Spain centuries ago. Among the Basque people there, 30 percent are Rh-negative — the highest concentration we’ve found anywhere.”
During his medical school lectures, Dr. Moise asks students to name five things Columbus brought to the New World. “Nobody ever mentions the Rh-negative blood type. But everything points to that,” he said.
In the three decades RhoGAM has been used, not a single case of viral disease transmission has been documented, according to Dr. Moise. He attributes that to careful screening of plasma donors, good manufacturing quality control and the capability of removing certain viruses during the production process.
The patented RhoGAM ultra-filtration process removes enveloped and non-enveloped viruses, including viruses that cause AIDS, hepatitis C and Fifth’s disease.
Dr. Moise said that while RhIG has been an overwhelming success in reducing HDF/N, he doesn’t believe the disease will ever be completely eradicated. “We’ve gotten it about as low as it’s going to get,” Dr. Moise said. Lack of proper prenatal care, misdiagnoses and oversights continue to be problems. In fact, there are countries around the world that have little or no supplies of Rh immune globulin.
Supply has also become an issue in Great Britain. Last year’s Mad Cow disease outbreak and other problems with human plasma there have led Britain to enact a moratorium on plasma-derived products. So the country depends on imports from the U.S. for its Rh immune globulin, which is under an effective state of rationing.
“The United States has been described as the OPEC of plasma in the world,” Dr. Moise said. “We have the best screening, the highest quality controls. The world depends on us.”
Another concern: the available supply of Rh-negative people to provide the plasma used in the production of Rh immune globulin. Successful treatment shrinks the number of Rh-negative women with antibodies; that means a reduced base of potential plasma donors. Attempts to develop a synthetic or monoclonal based RhIG product haven’t been proved safe, efficacious or cost-effective.
Given correctly, RhIG is more than 99 percent effective in the prevention of Rh disease. But this medication only prevents Rh disease; it is not effective, Dr. Moise said, in preventing worsening disease once alloimmunization occurs. Where a mother’s Rh antibody level is extremely high, treatment could require an intrauterine transfusion of red blood cells through the umbilical cord.
In recent years, Dr. Moise has pioneered several important developments in the management of alloimmunized pregnancy. These include the use of a patient’s own red blood cells to transfuse her fetus, a combined intrauterine transfusion technique and use of fetal blood pressure monitoring during transfusions to reduce fetal loss.
Despite success in reducing Rh disease, there is still much to be done in the management of red cell antibodies. Although the Rh D antigen is responsible for more than 98 percent of all HDF/N cases, Dr. Moise says, more than 43 other red cell antigens have been implicated.
Prominent among them is the Kell (K1) antigen. For this reason, according to Dr. Moise, Kell typing of the father is the primary step in the management of Kell disease in pregnancy.
Comprehensive prenatal care including early identification of women who are candidates for RhIG and appropriate treatment with RhIG in all scenarios that might lead to exposure of the mother to Rh-positive red cells are key factors in the prevention of alloimmunization and subsequent potential hemolytic disease of the newborn. Rh immune globulin is truly a success story.

Ovarian cancer is both silent and lethal. Every year in the United States physicians diagnose approximately 25,000 new cases of ovarian cancer, and about 15,000 deaths occur. Its symptoms are vague; it is all too easy for physicians to attribute abdominal swelling, pain, nausea, bloating and weight loss, to other, more common diseases. Consequently, diagnosis of ovarian cancer is typically delayed until more apparent symptoms, such as invasion or compression of nearby structures, ascites or metastases, occur. As a result, approximately two-thirds of women with ovarian cancer have advanced disease at the time of diagnosis. When ovarian cancer is diagnosed in the later stages, the five-year survival rate is below 30 percent. In contrast, early diagnosis and treatment is associated with a much more acceptable five-year survival rate of 95 percent.
Ovarian cancer is the most lethal of all gynecologic cancers, and is the fifth leading cause of cancer death overall. In contrast, uterine cancer can usually be successfully treated despite the lack of an early screening test, and cervical cancer survival rates have risen over the last 20 years, in part due to the availability of adequate early screening.
Still, researchers have made some advances in treating the disease and are aggressively seeking an effective screening tool for ovarian cancer. Although physicians can occasionally detect ovarian cancer by pelvic examination, the cancers found by this means are typically advanced. The PAP smear also occasionally reveals malignant ovarian cells; however, its sensitivity is only 10-30 percent, so it not considered a valid option. Transvaginal ultrasound has been considered as another possible screening option, but because the test is so sensitive it results in an inordinately high number of follow-up procedures and a low positive predictive value. Another screening option may be to measure women’s CA 125 antigen levels using a CA 125 tumor marker test.
A brief history of CA 125
The CA 125 tumor marker is found in the blood of many women with ovarian cancer. In the early 1980s, Robert Knapp, M.D., professor of gynecology at Harvard Medical School in Cambridge, Mass., co-developed a monoclonal antibody, which recognizes the antigen on the surface of an ovarian cancer tumor. Knapp explains, “The advantage of monoclonal antibody is the opportunity for both specificity and perpetuity.” Studies of the stored sera of women with known ovarian cancer have found that about half of the women had CA 125 levels over 35 U/mL 18 months to 3 years before their diagnosis.
The next step was to develop an assay to detect the ovarian cancer antigen in the blood serum. Eighty to 90 percent of women with advanced ovarian cancer have a CA 125 level over 35 U/mL. In the normal population, only 1 percent of people have a level over 35 U/mL.
During 1987, the FDA approved a CA 125 test for the intended use at the completion of primary therapy for ovarian cancer. The test is predictive of residual cancer if it shows that the woman’s CA 125 level is over 35. The test has also become standard medical practice in monitoring women with invasive epithelial ovarian cancer. Knapp says, “If the CA 125 level is rising during treatment it means there is progressive disease. It appears that this rise occurs before the disease can be detected clinically or radiologically. Moreover, if the level falls rapidly, it’s a good prognostic sign. If the level is below 35 for three months or more, it doesn’t mean there is no cancer. It does mean the patient is responding to chemotherapy, and it is a sign that chemotherapy is the correct program.”
Another use of the CA 125 test is to follow patients for recurrent ovarian cancer. The test is highly indicative of recurrent cancer if it shows a CA 125 level over 35 or if there is a longitudinal rise in the level after treatment.
A final utilization of the CA 125 assay is to help differentiate a benign mass from a malignant mass. If a physician feels an ovarian mass, he can combine CA 125 and ultrasound to determine whether or not the mass is malignant. The results allow the physician and patient to prepare for the appropriate surgical procedure.
A second generation CA 125 test, CA 125 II was approved by the FDA during 1992. With the development of the CA 125 II test, clinicians now have an improved method for measurement of the CA 125 antigen, most significantly at very low quantitative levels. According to Dr. Knapp, this next generation assay has greater accuracy with less variability. “The decreased variability with the CA 125 II assay is particularly important when looking at cancer recurrence, where consistency in measurements is vital. Changes in time are even more significant than high levels,” said Knapp. Decreasing the variability of assay performance, particularly at very low levels, allows for improved monitoring of disease.

CA 125 and ovarian cancer screening
Screening for any type of cancer can be a dicey business. Knapp says, “To say any screening test is effective it has to demonstrate a increase in the survival rate.” The current heated debate over the effectiveness of screening mammograms illustrates the precariousness of universal screening recommendations. Knapp affirms, “CA 125 II is not yet proven as a screening test.” That may change.
Knapp points to a large prospective evaluation underway at the University of London. The United Kingdom Collaborative Trial of Ovarian Screening (UKCTOCS) was launched in 2001. The study is the world’s largest-ever ovarian cancer screening trial and will screen 200,000 postmenopausal women over a 10-year period. The study is limited to postmenopausal women for a variety of reasons. Postmenopausal women face a higher risk of developing ovarian cancer than their premenopausal counterparts, and CA 125 levels may be elevated in premenopausal women for reasons other than ovarian cancer. Benign ovarian cysts, pregnancy or endometriosis can cause elevated CA 125 levels.
The UKCTOCS study will look at three variables: sensitivity, specificity and positive predictive value through three arms. For the first arm, the study’s investigators developed a risk of ovarian cancer algorithm and will divide women into three risk groups: low risk, intermediate risk and high risk depending on the results of the CA 125 test. Women who fall into the low risk category will undergo annual CA 125 tests. If an initial CA 125 test determines that a woman is at intermediate risk for ovarian cancer, her physician can opt to repeat the test in one month or perform an ultrasound. If the CA 125 test shows that a woman is at high-risk for ovarian cancer, the physician can opt for either surgery or transvaginal ultrasound. The second arm of the study will compare CA 125 testing to transvaginal ultrasound alone. Ultrasound alone tends to be very sensitive and pick up minor abnormalities that are not ovarian cancer. The third arm of the study is a control group. Knapp says, “Considering the fact that ovarian cancer is a relatively difficult disease to diagnose and it has a poor survival rate, a positive predictive value over 10 percent is acceptable for ovarian cancer.” Knapp is optimistic about this possibility. A study published in 1999 in The Lancet found that screening with CA 125 had a positive predictive value of 20.7 percent if 30 U/mL or more was used as the cutoff for ultrasound referral.
Complementary testing?
CA 125 is the only available blood test for ovarian cancer at this point; however, other tests for other proteins associated with ovarian cancer may be coming down the pike. The combination of CA 125 with another test may be the most effective ovarian cancer screening mechanism. But for a blood test to be considered effective, it must meet stringent demands. It should have a specificity of 99.7 percent and sensitivity over 80 percent. With a combination of two tests, if either test were positive sensitivity would improve, and if both tests were positive specificity would improve.
The CA 125 test can be performed on the Vitros ECi Immunodiagnostic System with Intellicheck, using Ortho-Clinical Diagnostics’ CA 125 II assay with patented Fujirebio antibodies. The Vitros CA 125 II assay is to be used as an aid in monitoring response to therapy for patients with epithelial ovarian cancer. Serial testing for patient CA 125 assay concentrations should be used in conjunction with other clinical methods used for monitoring ovarian cancer.

Americans today are largely able to take for granted the availability of safe and effective birth control methods. But what about the other side of the family planning story —infertile couples who want children?
According to Dr. Thomas Pool, Ph.D., embryologist and scientific director at the Fertility Center of San Antonio, reproductive medicine—especially assisted reproductive technology—has become today’s most active subdiscipline of obstetrics and gynecology in terms of research activity, technology development and public interest.
About 6 million Americans — 1 of every 10 in the reproductive age population — face infertility problems at some time in their lives. The state of a person’s overall health is no indicator of fertility problems. Usually, infertility is diagnosed only after repeated failures by couples to conceive or bring a pregnancy to term. For women, regular menstrual cycles and a clean gynecological bill of health are not enough.
Infrequent or irregular ovulation, decreasing egg quality brought on by age, blocked or scarred fallopian tubes and endometriosis are common causes of female infertility. For men, low sperm count, poor sperm motility, abnormally shaped sperm or some combination are the most frequent villains.
Conception depends on many factors: healthy sperm and healthy eggs, unblocked fallopian tubes that host the sperm’s trip to the egg, the sperm’s ability to fertilize the egg, the quality of the fertilized egg and its ability to implant in the woman’s uterus.
For a full term pregnancy, the embryo must be healthy and the woman’s hormonal environment must be sufficient for the embryo’s growth. Infertility can result when any one of these factors is impaired. An elevated level of follicle stimulating hormone (FSH) in a woman is an indication of reproductive aging. That suggests a woman is producing fewer eggs and eggs of diminished quality.
The Society for Assisted Reproductive Technology (SART), an affiliate of the 9,000-member American Society of Reproductive Medicine, has about 300 member in vitro fertilization programs in the United States.
Dr. Pool says the two most important issues facing infertile couples are the cost of treatment and stress related to a failure to conceive. While a few states do mandate insurance coverage for infertility treatments, most patients are faced with paying for fertility therapy out of pocket. And the cost of technology in science and medicine is substantial. “Patients are typically paying in the neighborhood of $10,000 for a single attempt at achieving pregnancy with in vitro fertilization,” Dr. Pool said. Most Americans, meanwhile, believe that health care coverage should include the costs of infertility treatments.
In the last 22 years in the U.S., more than 45,000 babies have been born through In Vitro Fertilization (IVF); over 70,000 more babies have come into the world with the aid of assisted reproductive technologies. The average live delivery rate for IVF was 22.5 percent in 1995, nearly the same as the 20 percent chance in any given month that a reproductively healthy couple has of getting pregnant and carrying to term. Still, in vitro fertilization and related treatments account for less than 5 percent of infertility services.
Perhaps the most significant determinant of success, according to Dr. Pool, is maternal age and associated ovarian reserve. The “ticking biological clock,” financial burden, and invasion of marital privacy all unite to push up stress levels among infertile couples.
For the average woman, fertility begins to decline well before her late 30s and early 40s. The most up-to-date study suggests the decline begins in her late 20s. Typically, the average number of cycles required for conception to occur increases substantially after age 27.

Major Steps Forward
Fertility drugs produced through recombinant DNA technology (rather than human-derived products) have improved both the safety and reproducibility of ovulation induction in women seeking pregnancy.
“Improving culture systems and culture media now provide for the routine propagation of late-stage human embryos (blastocysts). The transfer of blastocysts instead of younger, cleavage-stage embryos has maintained excellent pregnancy rates while simultaneously reducing the incidence of high order multiple gestations, such as triplets,” according to Dr. Pool.
He said new surgical methods for obtaining testicular biopsies (related to successful injecting of single spermatozoa into oocytes) can result in pregnancies in cases of severe male factor — something that could not have been treated just a few years ago. To overcome known familial genetic disorders, new techniques for pre-implantation genetic diagnosis (PGD) enable the selection of genetically normal embryos for transfer.
Central to diagnosing ovulatory disorders and monitoring medical therapy of ovulation induction is a reliable endocrine assay system. Highly sensitive and consistent assays for follicle stimulating hormone (FSH), estradiol and progesterone are a prerequisite for successful fertility therapy.

Reliable Hormone Data Rapidly
“The assays offered by Ortho-Clinical Diagnostics are reliable and repeatable,” Dr. Pool said. “The platform is user-friendly and, most importantly, fast. Since we use the hormone data to individualize patient treatment dosages on a daily basis, it is imperative that hormone assays be rapid and reliable. Patients rely upon us for success and we, in turn, rely upon Ortho to help us deliver quality care.”
Finally, becoming pregnant — even for the most fertile couples — can require patience, said Dr. Pool. With an average rate of pregnancy in the general population of approximately 20 percent per menstrual cycle, it may take a year of trying to conceive naturally.
“Infertile couples must also be prepared to be patient,” Dr. Pool said. “The good news is that the vast majority of our patients ultimately conceive, if they do not postpone therapy too long and if they stay in the game long enough to let the mathematics of reproduction work for them.”