The US Preventive Services Task Force (USPSTF) has published a final recommendation on risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women. USPSTF recommends that women who have a family history of certain types of cancer—or who have an ancestry associated with BRCA1 or BRCA2 mutations—should be assessed for increased risk of BRCA1 or BRCA2 genetic mutations.1 Women who are found to be at increased risk should receive genetic counseling and, if indicated after counseling, BRCA testing. This is a B recommendation.
Women who do not have a family history or ancestry associated with a mutation should not undergo risk assessment, genetic counseling, or testing. This is a D recommendation.
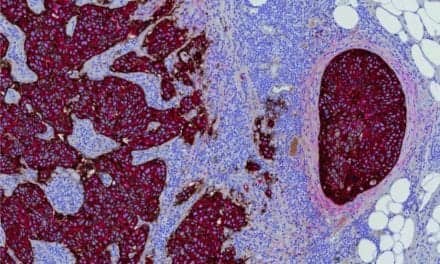
BRCA1 and BRCA2 genes produce proteins that repair damaged DNA and, as a result, help lower a woman’s likelihood of getting certain cancers. When either of the BRCA genes is mutated, cells in the body are more likely to develop additional genetic changes, or mutations, that can lead to breast, ovarian, peritoneal, and other cancers. Fewer than 1% of all women have a mutation in either of the BRCA genes.
The task force’s recommendation lays out the steps women can take to determine whether they are potentially at increased risk for BRCA gene mutations. The first step is talking to a clinician about their personal or family history or ancestry to see if a risk assessment is needed.
“There are several steps women can take to find out if they are at increased risk for BRCA gene mutations and if genetic counseling and BRCA testing is needed,” says task force member Carol M. Mangione, MD, MSPH. “Women who have a personal or family history of certain types of cancers, or have ancestry associated with the BRCA mutations should discuss their risk with their clinician and, if indicated, undergo counseling and potentially genetic testing. Because these tests are not without harms, testing for BRCA mutations in women without these risk factors is not recommended.”
In some cases, women may only get a risk assessment and receive counseling. For example, a woman may get a risk assessment and, after a discussion with a genetic counselor, decide she would not benefit from getting tested. Testing should be done only after a woman has discussed the benefits and harms of testing with a trained health professional. The test results cannot always tell a woman if she has a potentially harmful mutation that could lead to cancer.
“Some women can benefit from risk assessment, counseling, and testing, but not all women need these services,” says task force chair Douglas K. Owens, MD. “We suggest women talk to their clinicians and decide on the best next steps together.”
USPSTF is an independent, volunteer panel of national experts in prevention and medicine that works to improve the health of all Americans by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications.
Mangione is chief of the division of general internal medicine and health services research, and holder of the Levey chair in medicine at the David Geffen School of Medicine at the University of California, Los Angeles. Owens is a general internist and investigator at the center for innovation to implementation at the Veterans Affairs Palo Alto Healthcare System, and a professor of medicine at Stanford University.
Myriad Genetics, Salt Lake City, announced its support of the USPSTF recommendations.
“We applaud USPSTF for recommending hereditary cancer risk assessment for all women with a family or personal history of certain types of cancers or who have an ancestry associated with BRCA mutations,” says Royce T. Adkins, MD, FACOG, a board certified obstetrician-gynecologist and senior vice president for medical affairs at Myriad Women’s Health. “There are more than 3.5 million breast cancer survivors who see their OB/GYN or primary care doctors annually. The valuable information provided by hereditary cancer risk assessment can help clinicians select appropriate precision treatments, customize treatment plans, and achieve better health outcomes for their patients.”
Myriad’s myRisk Hereditary Cancer test is a leading test for patients trying to understand their cancer risk. The Myriad test uses an extensive number of sophisticated technologies and proprietary algorithms to evaluate 35 clinically significant genes associated with eight hereditary cancer sites including breast, colon, endometrial, ovarian, pancreatic, and prostate cancers.
The new USPSTF recommendations reflect a growing trend among medical experts to expand hereditary cancer risk assessment and genetic testing for more people at risk. In February 2019 the American Society of Breast Surgeons updated its guidelines on genetic testing, recommending that it be made available to all newly diagnosed patients with breast cancer.
According to the American Cancer Society, 330,000 people are diagnosed with breast cancer annually in the United States, and an estimated 10% of those cases are caused by inherited mutations. Fewer than 10% of individuals with BRCA1 or BRCA2 mutations have been identified, and up to 80% of individuals at risk have not received genetic testing.
For more information visit the US Preventive Services Task Force.
Reference
- BRCA-related cancer: risk assessment, gene counseling, and genetic testing [final recommendations summary, online]. Rockville, Md: US Preventive Services Task Force, 2019. Available at: www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/brca-related-cancer-risk-assessment-genetic-counseling-and-genetic-testing1?ds=1&s=breast%20cancer. Accessed September 30, 2019.