Men with a particular genetic subtype of the steroid biosynthesis enzyme biomarker HSD3B1 may exhibit resistance to combined radiation and hormone therapy for prostate cancer, according to new Cleveland Clinic-led research published in Journal of Clinical Investigation.
Historically, there has been a lack of reliable biomarkers to predict response to combined hormone therapy and radiotherapy, a standard treatment for high-risk prostate cancer. The enzyme encoded by the gene HSD3B1 is a potential predictive biomarker that may aid clinicians in determining up front whether a patient with prostate cancer may benefit from intensified hormone therapy combinations, such as adding an androgen receptor selective inhibitor (ARSI) to conventional treatment.
Cleveland Clinic researchers had initially described germline variants in the biomarker HSD3B1 gene, one of which led to more rapid resistance to androgen-deprivation therapy. Building on this work, the team studied whether or not this HSD3B1-mediated partial or complete resistance to hormone therapy promotes radiotherapy resistance as well in men with localized, potentially curable disease.
“The stability of the enzyme can dramatically influence the rate at which tumor cells produce testosterone from circulating adrenal precursors, which is critically important for a disease like prostate cancer that is driven by testosterone,” says study co-author Omar Mian, MD, PhD, a radiation oncologist and physician-scientist at Cleveland Clinic. “The adrenally permissive allele of HSD3B1 can increase the production of testosterone in tumors, bypassing the most commonly used class of testosterone-lowering medications, with the downstream effect of promoting resistance to combined hormone therapy and radiation”.
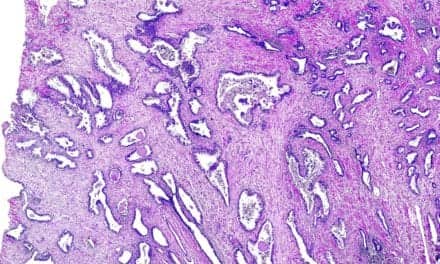
This pre-clinical and mechanistic study sought to evaluate whether levels of 3βHSD1 (the enzyme encoded by biomarker HSD3B1) were associated with radiation resistance. In addition, the study team aimed to determine the precise mechanism for this resistance. Researchers evaluated preclinical models of prostate cancer and specifically examined their level of radiation response.
They also explored the influence of 3βHSD1 levels and HSD3B1 genotype on DNA damage repair capacity of prostate cancer cells. They examined the association between androgen signaling and DNA repair pathways in 681 patient samples treated for prostate cancer at Cleveland Clinic for whom there was gene expression data available. Finally, they attempted to reverse the 3βHSD1 mediate radio-resistance with targeted hormone therapy combinations.
“There was a clear association between androgen receptor signaling and DNA damage response across the preclinical models as well as patient samples,” says Mian. “Even low-level testosterone production in the tumor itself, and presumably the region around the tumor, appeared to drive a robust resistance to radiotherapy. This resistance was associated with an enhanced DNA damage repair capacity in cells expressing the adrenally permissive subtype of 3βHSD1.” Importantly, the study team found that this resistance was reversible by treatment with direct androgen receptor targeting therapy with an ARSI.
The researchers are now conducting a prospective registry of the HSD3B1 genotype to validate the study findings in patients receiving combined radiation and hormone therapy. The center is enrolling patients with high-risk, localized disease and low-volume metastatic disease, for whom radiotherapy to the prostate combined with androgen-deprivation therapy is a standard of care. The main clinical implication of this work is that a germline biomarker may identify a high-risk subset of men who would benefit from targeted therapies combined with conventional hormone therapy and radiation.
These studies may lead to routine use of genotyping of enzymes like biomarker HSD3B1 to risk stratify patients and match them to the appropriate treatment. This could result in intensifying treatment for patients with high-risk disease, or scaling back treatment for patients who harbor a less aggressive genetically-defined variant of prostate cancer, to spare them the side effects of more intense treatment.
“With diseases like prostate cancer that have a wide spectrum of aggressiveness, biomarkers that can help us to more precisely match patients to the most appropriate treatment are important,” says Mian.