Pooled testing addresses the problem of having too few test kits available
By Milan Patel
As the outbreak of the novel coronavirus SARS-CoV-2 spread rapidly across the globe, attaining pandemic status at the beginning of February, it soon became evident that the world’s healthcare systems were unprepared to contain or control the virus.
Slow responses and inadequate availability of test kits and related supplies led nations to abandon containment strategies and employ mediation through ‘social distancing’ as their primary means of responding to the outbreak. In turn, such actions have effectively shut down much of the global economy, causing widespread fear and anxiety and highlighting the need for a more effective approach.
From the beginning of the outbreak, testing has been at the center of the storm. With too few test kits available, testing was initially restricted to people with symptoms of the novel coronavirus disease-2019 (covid-19), or those thought to have been exposed to the virus. And just as the supply of reverse transcription polymerase chain reaction (RT-PCR) tests suitable for making diagnoses was beginning to catch up with that need, a new need arose for tests to confirm whether individuals had developed antibodies after exposure to the virus.
The presence of antibodies is thought to be the best indicator of potential immunity to the SARS-CoV-2 virus—though there is scant evidence to confirm that antibodies convey such immunity, or to suggest how long such immunity might last. But yet again, clinical labs have been frustrated by the unavailability of antibody tests, as well as by the poor quality of many such tests that have found their way to market in a period of regulatory discretion.
Whether they are seeking to diagnose patients through the use of molecular testing, or to gauge patients’ potential immunity through antibody testing, labs are unable to make progress without access to sufficient quantities of the test kits and other supplies that make testing possible. But with an entire planet’s population eager to be tested, the number of available tests seems likely to be forever inadequate to the task.
Into the Pool
Pooled testing offers a potential solution to the problem of having too few kits available to test everyone who wants or needs to be tested. The method involves testing patient samples in batches, or ‘super samples,’ to detect the presence of the SARS-CoV-2 coronavirus. When creating a batch, only ¼ of each patient’s sample is used, leaving a reserve for subsequent reflex testing at the individual level. If the batch tests negative, then all of the samples that made up the batch can also be considered negative. If the batch tests positive, then each of the contributing patients’ samples must be tested independently to determine which of the patients’ samples is positive for the virus.
Pooled testing offers a variety of benefits to labs, providers, and patients alike. The pooled approach speeds testing in order to clear the backlog that develops when tests cannot be processed in a timely manner. Speedier testing also helps to free up the lab’s testing capacity, and reduces the time between sampling and delivery of results. Additionally, pooled testing eases the burden on testing centers by cutting the need for individualized testing, thereby reducing the lab’s use of kits and reagents—as well as the costs associated with such use.
Pooled testing makes it possible to communicate positive test results more quickly—especially important for presymptomatic or asymptomatic individuals—so that the spread of the disease can be reduced by getting people into quarantine sooner. Public health officials can then track infected individuals’ contacts sooner. And delivering negative results earlier may reduce individuals’ anxiety over whether they are ill or contagious.
Pooled testing is not appropriate for all situations. In populations where the infection rate is believed to be greater than 3%, it is economically efficient to test individuals independently, on a one-by-one basis. In such ‘hotspot’ areas, the virus is spreading so rapidly that pooling becomes a waste of time. It can be assumed that each pooled batch would yield at least one positive result, meaning that the entire sample would require individual testing.
Nevertheless, in populations where the infection rate is below the 3% threshold, pooling provides the opportunity to test millions of people with just a fraction of the time, cost, and effort that would otherwise be required.
Real-World Efforts
International researchers are examining pooled testing as a means of slowing the spread of covid-19. In one experiment, scientists of the Rambam Medical Center and the Technion in Haifa, both in Israel, performed pooled testing with samples of up to 32 and 64 people at a time, and found that the test could yield a positive result even if just one member of the group was positive for covid-19.1
In a separate effort, researchers at the German Red Cross blood donor service and the institute for medical virology at University Hospital Frankfurt conducted a field study with 50 patient samples divided among 10 mini-pools of five samples each.2 The 50 individuals were also tested separately in parallel. Of the 50 patient samples, five came back positive, distributed across four of the mini-pools. Mini-pools containing only negative samples always came back negative.
India is also looking to embrace the pooling method, not least because of the sheer size of the country’s population and its low ratio of doctors to patients.3 Norms established by the World Health Organization recommend that there should be one doctor for every 1,000 persons. But in rural India, the ratio is as low as one doctor for more than 10,000 patients. Such a mismatch of medical resources emphasizes the need for efficient testing.
In the United States, the response of the medical community to the covid-19 pandemic is also suffering from inefficiency, in part because of the country’s large geographical size and the uneven distribution of its population, but also because of the multiplicity of decentralized government and private entities responsible for providing patient care. Pooled testing can help to get the country back on track.
Early examples of pooled testing in the United States include research conducted at the Stanford Healthcare clinical virology laboratory, where investigators screened 292 pooled samples comprising 2,888 individual samples.4 Although the pooled samples of this study returned one false-positive result, the authors continue to favor pooled testing as a means of simultaneously screening multiple individuals who are asymptomatic or do not fit the covid-19 screening guidelines of recent travel or known exposure.
In another US study, researchers at the Nebraska Public Health Laboratory found that pooled testing of five samples at a time resulted in a 58% reduction in the number of test kits used, correlating to a 137% increase in tested individuals.5
Some regions have moved ahead with use of pooled testing. Pooled samples were used early in the outbreak to trace community transmission of covid-19 in the San Francisco Bay Area.6 And Nebraska was for a time using pooled samples, until its rate of positive tests jumped above 10%—a threshold that required a return to individual testing.7
To the Rescue
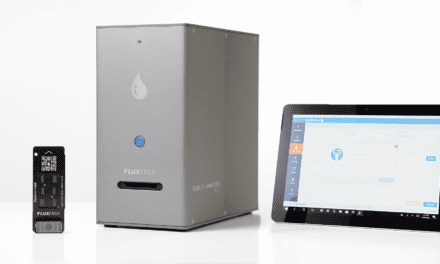
To facilitate pooled testing for covid-19, PathogenDx offers two test kits. The DetectX-Rv kit is a human diagnostic that uses a nasopharyngeal swab specimen to test for covid-19. The EnviroX-Rv kit tests for covid-19 in the air and on surfaces in the environment (Sidebar 1).
The PathogenDx technology is a two-step polymerase chain reaction (PCR) test with DNA hybridization on a multiplexed microarray platform. The full test suite comprises a turn-key equipment set; reagent kits that can test for the SARS-CoV-2 coronavirus through individualized testing, pooled testing, or environmental air and surface contamination testing; and Cloud-based analytical software for reporting results.
With the PathogenDx technology, individual nasopharyngeal samples are collected and separated into groups of 10 to create batched ‘super samples.’ Results are returned within 24 hours—a time savings of 3 to 4 days over the current average turnaround time at large central processing labs.
Relative to the cost per sample of covid-19 testing with standard RT-PCR techniques, the cost per sample of testing with the PathogenDx technology is roughly 10% to 15% less expensive. But when pooled for a family of four, the PathogenDx technology generates a savings of 66%. Spread across a community with a population of 10,000 or more, the savings to the healthcare system can be significant.
PathogenDx’s DetectX-Rv ultrarapid multiplex pathogen screening panel can test not only multiple patient samples, but also for multiple disease markers (Figure 1). In addition to testing for covid-19, the pan respiratory viral panel detects the coronavirus pathogens that cause Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), other coronavirus variants, influenza types A and B, and norovirus. Using a single nasal swab sample, results for all of these markers can be returned in 6 hours.
Now and Future Use
Covid-19’s march across the globe has been aided by the international dearth of test kits and efficient testing systems. The need for covid-19 testing methods that provide rapid results using few resources remains critical. But even beyond the current moment, cost-effective methods for covid-19 testing will remain essential to keep the virus in check until a vaccine is developed. And even with a vaccine, covid-19 will remain a threat, especially to high-risk individuals.
Until a reliable and effective vaccine has been developed, there will be an ongoing need for cost- and time-efficient solutions to keep outbreaks in check and to prevent future contagion. Maximum efficiency will come from a testing system that enables healthcare providers to screen for multiple viruses concurrently.
Pooled sample testing, such as that offered by PathogenDx, provides an option for returning multiple results quickly, helping individuals and health officials to contain the spread of covid-19. l
Milan Patel is CEO of PathogenDx.
REFERENCES
1. Jeffay N. To ease global virus test bottleneck, Israeli scientists suggest pooling samples. The Times of Israel. March 18, 2020. Available at: www.timesofisrael.com. Accessed April 27, 2020.
2. Corona ‘pool testing’ increases worldwide capacities many times over [online]. Healthcare in Europe. Epub updated January 4, 2020. Available at: https://healthcare-in-europe.com/en/news/corona-pool-testing-increases-worldwide-capacities-many-times-over.html#. Accessed April 27, 2020.
3. India assesses covid-19 sample pooling for tests, says top scientist. How it helps. Hindustan Times [online]. Epub updated March 30, 2020. Available at: www.hindustantimes.com/india-news/india-takes-cue-from-israel-to-use-pooling-method-to-test-samples-for-covid-19/story-IFriWFUaLKR8euVT5WpQTM.html. Accessed April 27, 2020.
4. Hogan CA, Sahoo MK, Pinsky BA. Sample pooling as a strategy to detect community transmission of SARS-CoV-2. JAMA. 2020;323(19):1967–1969; doi: 10.1001/jama.2020.5445.
5. Bilder CR, Iwen PC, Abdalhamid B, Tebbs JM, McMahan CS. Increasing testing capacity for SARS-CoV-2 by pooling specimens. Significance [online]. Epub April 9, 2020. Available at: www.significancemagazine.com/science/651-increasing-testing-capacity-for-sars-cov-2-by-pooling-specimens. Accessed April 29, 2020.
6. Broadfoot M. Coronavirus test shortages trigger a new strategy: group screening [online]. Scientific American. Epub May 13, 2020. Available at: www.scientificamerican.com/article/coronavirus-test-shortages-trigger-a-new-strategy-group-screening2. Accessed May 26, 2020.
7. Anderson J. Group testing for covid-19, used in Nebraska, seen as ‘promising way’ to conserve testing supplies [online]. Omaha World-Herald. May 25, 2020. Available at: www.omaha.com/livewellnebraska/group-testing-for-covid-19-used-in-nebraska-seen-as-promising-way-to-conserve-testing/article_123ac7d8-7b85-58bc-b12d-a52f855d530d.html. Accessed May 26, 2020.