By Nicholas Borgert

Pathologist Jared Schwartz, MD, PhD, says the Centers for Disease Control and Prevention and US public health officials responded well to this year’s outbreaks of SARS and monkeypox. “Of course, we had very few cases in the United States. We were not challenged as Toronto was,” Schwartz says.

Schwartz says he doesn’t believe this country is adequately prepared to respond to a serious bioterrorism attack. “I think public health is geared up to deal with such a crisis,” he says, “but community physicians and local hospital emergency rooms are not. Mentally, they may be ready, but their first response would be to send a patient to the emergency room. That’s exactly what we don’t want. We don’t have the necessary health care infrastructure.”
Because Toronto had 15 hospitals in the area, officials were able to respond to their SARS outbreak by closing four and using them to isolate patients—the only known SARS treatment now. Few American cities are so fortunate. And maintaining preparedness can be very expensive. “I think there’s a reluctance to spend a lot of money. Complicating that, we tend to underestimate how much such an event will cost,” Schwartz says.
As for SARS and health worker safety, Schwartz says existing gear such as gowns, gloves, and masks can markedly reduce risks, provided workers use them consistently and appropriately. “But behavior modification can be a difficult thing, even among physicians and lab staff who should know better,” he says.
Moving Approvals Along
On the regulatory front, a year ago, the FDA created the new Office of In Vitro Diagnostic Device Evaluation and Safety. Donald St. Pierre, its deputy director, says his office takes a life-cycle approach. It attempts to better balance premarket and postmarket activities.
“We’re looking at products to see how we can regulate them differently and more effectively,” St. Pierre says. Working with PANBIO on the first test for West Nile Virus, the office was able to expedite the process and get approval of the test in a week. “That’s pretty significant for a first-time product,” says St. Pierre.
His office has worked hard to increase cooperation with other agencies within Health and Human Services. For example, it fast-tracked a clinical study protocol for a new SARS test developed by the CDC. “We were heavily involved up front with that,” St. Pierre says. “As a result, we were able to grant an Investigational Device Exemption (IDE) and approve the study in less than 48 hours.”
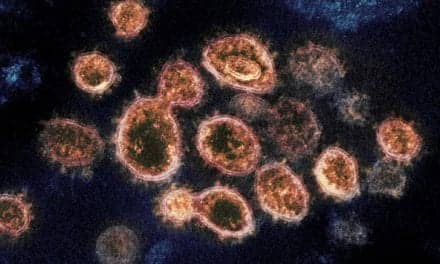
The CDC has distributed its experimental SARS diagnostic test to about 100 laboratories across the United States. The test was developed over a few months and is now undergoing field trials. The standard method–growing the organism in cell culture–requires several days to several weeks for results. Results from the new CDC test, according to reports, are available in a couple of hours.
Finally, new user fees have improved the FDA’s IVD service. “With our Web site and other educational efforts, we’ve made IVD more visible, more reliable as a resource,” St. Pierre says. “With new user fees, we’re able to hire an additional 12 people. That’s a major improvement.”
Focus Technologies
Mary Kay Mosch, vice president of marketing at Focus Technologies, says FDA efforts to streamline approvals are making an impact. “We noticed the difference when working with the Office of In Vitro Diagnostic Device Evaluation and Safety about our WNV IgG and IgM ELISA 510(k) clearance,” Mosch says. “It does streamline the submission process.”
Infectious diseases have been the core of Focus Technologies’ business for all its 25 years. In response to outbreaks of SARS, Focus offers SARS culture and a polymerase chain reaction (PCR) assay as a service within its reference laboratory, Mosch says.
While Focus does not currently market any SARS diagnostic products, Mosch says, efforts are under way to offer SARS serology as a laboratory service in the future. The Focus system detects the genomic RNA from the coronavirus through reverse transcription of specific viral genomic RNA and PCR amplification. Results are usually available within 72 hours.
The newest Focus product line is aimed at West Nile Virus IgG and IgM antibody detection. Early in 2003, Focus started selling analyte specific reagents (ASRs) for WNV. “Today our IgG and IgM WNV products are in the FDA review process,” Mosch says. “Market demand for these products is very high from all market segments — public health, commercial laboratories, and hospitals.”
Concerns about the West Nile Virus have also prompted increased demand for the company’s Arbovirus IgG and IgM products. Another high-growth area is its line of HerpeSelect Type 1 and HerpeSelect Type 2 products in Immunoblot and ELISA formats. Mosch describes the products as the only HSV type-specific, FDA—cleared products on the US market today.
Recent estimates suggest more than 60 million people in the United States are infected with HSV-2, yet as many as 90% of them don’t know they have it.
HerpeSelect, Focus believes, will play a key role in driving increased diagnosis of this disease.

Focus has also been a busy partner with others. Mosch says the company recently entered into a semiexclusive agreement with ViroNovative BV to become the first US lab to license ViroNovative’s rights to nucleic acid diagnostic testing for human metapneumovirus (hMPV). Human metapneumovirus is a newly discovered human viral respiratory pathogen that causes a spectrum of respiratory symptoms, ranging from asymptomatic infection to severe bronchitis.
In 2001, a team of scientists isolated the human metapneumovirus from young children with respiratory disease. Using banked sera, they determined the disease has been present in Europe—though unrecognized—for more than 50 years.
Crucell
Even though Crucell is headquartered in the Netherlands, the company sees the US market as vitally important, says Domenico (Dinko) Valerio, PhD, its president and CEO. Valerio says Crucell’s association with investors, customers, and the FDA is essential to the company’s long-term success.
Traded publicly on NASDAQ, Crucell is the result of a merger in 2000 of two Dutch companies: IntroGene BV and U-BiSys BV. The company has effectively extended products using the PER.C6 human-cell–based platform introduced by IntroGene and by leveraging the antibodies expertise of U-BiSys.
Besides directing Crucell, Valerio is a professor of gene therapy at the University of Leiden. A postdoctoral fellow at the Salk Institute and once a visiting scientific specialist at Genetech Inc, Valerio helped found IntroGene in 1993 and served as its first president and CEO. The company has responded to the industry’s dramatic shortage of antibody manufacturing with its own higher-yield system.
Crucell officials say they are the only firm developing a whole-killed virus vaccine against West Nile Virus infections for humans. The company is also developing a WNV vaccine for animals in collaboration with Kimron Veterinary Institute in Israel. Kimron’s current WNV veterinary vaccine has been used on upward of 800,000 geese and is derived from the brains of newborn mice. Geese are considered one of the best animal models for the disease. Following trials of Crucell’s WNV vaccine on geese, Kimron decided to pursue registration of Crucell’s WNV vaccine for animals to replace its existing vaccine.
It has finished one phase of preclinical studies with geese. In the trials, the experimental compound provided complete immunity to more than 90% of the geese challenged by a lethal injection of WNV. All geese in the control group died. The company is now involved in scheduling human testing.
While the industry’s focus has been on animal-based platforms, Valerio says, the Crucell PER.C6 human-cell–based platform is proving effective for large-scale, extremely pure vaccine production. Whole-killed vaccines are a widely used means for stimulating the body to produce antibodies to fight off an invading virus. Because the virus is killed in the vaccine production process, no disease is passed to the patient.
In addition, Crucell is working on an Ebola virus vaccine with cooperation from the US Army and National Institutes of Health (NIH). Initially, the vaccine would be stockpiled in case of a possible bioterrorist attack, Valerio says. That vaccine would be trialed under the FDA’s new “2 animal rule” and not subject to Phase III human trials. That will reduce the time to licensure for the product, he says.
The PER.C6 platform is proving valuable as Crucell eyes the $1.2 billion flu vaccine market. Valerio says traditional flu vaccines use decades-old technology based on embryos in chicken eggs. That technology is plagued by low yields—only three dosages per egg. But Crucell—using human cells to produce the vaccine—will deliver significantly higher yields at a competitive cost, Valerio says. He expects the new flu vaccine to enter clinical trials in 2005.
Nicholas Borgert is a contributing writer for Clinical Lab Products.