Amid increasing disease prevalence, new approaches seek to stem the tide
By Craig C. Foreback, PhD
With the prevalence of diabetes continuing on an upward trajectory both in the United States and overseas, healthcare professionals are continuing to search for more effective methods of preventing, detecting, and treating the disease. And as is often the case, clinical laboratories find themselves at the forefront of the effort, with their hands on the latest technologies. But just as often, being on the front line also means that labs are among the first to understand new problems as they arise.
In recent years, for instance, it has been recommended that hemoglobin A1c (HbA1c) be used to screen for diabetes. It is assumed that all glycated hemoglobin methods are equal, because most of them have been certified by the National Glycohemoglobin Standardization Program (NGSP). However, some methods—especially some point-of-care methods—do not have adequate precision to meet the demand.
A similar set of difficulties arises from the fact that immunoassays and affinity methods do not actually measure HbA1c, but in reality measure total glycated hemoglobin. Manufacturers label their methods as reporting HbA1c regardless of methodology, but that only means that they are traceable to an HbA1c calibrator. In patients with hemoglobin variants, glycated hemoglobin can be underestimated if the life span of the red blood cell is altered.
While dealing with such issues in the current generation of tests, laboratorians also have an eye on new diagnostics that are just appearing on the horizon. Capillary zone electrophoresis is now available for the analysis of HbA1c. Researchers have developed a plasmonic chip that can measure markers capable of distinguishing type 1 from type 2 diabetes. And adiponectin is a new assay that is being evaluated for assessing the risk of developing type 2 diabetes. In this article, we’ll take a look at these recent developments, and more.
TYPES OF DIABETES
Type 1 diabetes is an autoimmune disease that causes destruction of the pancreatic beta cell, leading to absolute insulin deficiency. Type 1 accounts for about 5% of all diabetes in the United States and does not appear to be increasing.
Type 2 diabetes results from a progressive secretory defect in the presence of insulin resistance. It is associated with increasing age, obesity, and physical inactivity. It is more prevalent among certain ethnic groups, such as African Americans, Hispanics, and Native Americans. Asians are generally at lower risk.
Prior to 1980, type 2 diabetes was rarely seen in children and adolescents. Since that time, however, the incidence of type 2 diabetes in young people has been increasing rapidly. Between 2002 and 2005, 3,600 cases were seen.1–3
[reference id=”39786″]Sidebar: Diabetes, by the Numbers[/reference]
Gestational diabetes is a form of glucose intolerance that occurs during pregnancy, affecting about 4% of pregnant women. If not treated, it can result in fetal complications. While it usually recedes following delivery, the presence of gestational diabetes is a risk factor for the mother developing type 2 diabetes later in life.
Testing for gestational diabetes is critical, and requires glucose tolerance testing with up to four collected samples. Since laboratories no longer routinely handle such requests, it is imperative that the samples be reported in a timely manner—and in the correct order.
RISK FACTORS AND COMPLICATIONS
“Metabolic syndrome” is a term commonly used to define health risks for a number of disorders that include diabetes. It is a disorder of energy utilization and storage, diagnosed by the coincidence of three out of five of the following medical conditions: abdominal (central) obesity, elevated blood pressure, elevated fasting plasma glucose, high serum triglycerides, or low high-density cholesterol (HDL) levels.
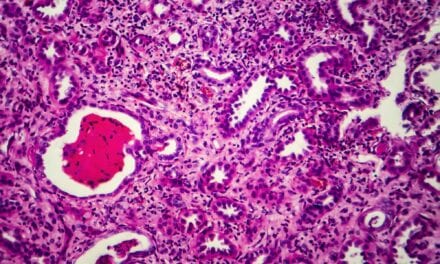
Diabetes affects all major organs through its effects on the vascular system. Retinopathy, neuropathy, and nephropathy are the most common complications of diabetes. Diabetes is the leading cause of blindness in adults.
Diabetes is also the most common cause of kidney failure.4 Even when diabetes is controlled, the disease can lead to chronic kidney disease (CKD) and kidney failure. In 2010, it was estimated that nearly 24 million people in the United States had diabetes, and nearly 180,000 people were living with kidney failure as a result of the disease.5 Fortunately, most people with diabetes do not develop CKD that is severe enough to progress to kidney failure.
Nervous system damage leads to impaired sensation in the hands or feet. Among long-term diabetics, 65% have nerve damage, and 30% of those over 40 have impaired sensation in their feet—a leading cause of lower-extremity amputations.6
More than half of all nontraumatic lower-limb amputations occur in diabetics. People living with diabetes are two to four times more likely to die from heart disease or stroke. More than 75% of diabetics are hypertensive, which is interesting, since 27% of the incidence of CKD is caused by high blood pressure.1
DIAGNOSING DIABETES
Diagnosis of diabetes has traditionally been based on blood glucose criteria, with tests using either a fasting or a 2-hour postprandial specimen. A fasting level of 126 mg or greater on two occasions, or a 2-hour postprandial value of 200 mg or greater on two occasions, has traditionally been considered diagnostic. A glucose tolerance test is recommended to diagnose gestational diabetes.
As an alternative to the traditional approaches for diagnosing diabetes, the clinical utility of hemoglobin A1c (HbA1c) was recognized as early as the 1980s. However, early methods for measuring HbA1c had wide variability (an issue that still persists), so adoption of standardized HbA1c values for diagnosis took many years to develop. Finally, in 2009, an international expert committee recommended the use of HbA1c to diagnose diabetes.3 The American Diabetes Association adopted the method in 2010. Nevertheless, confirming the notion that methods variability can still be an issue, a recent paper tested seven point-of-care HbA1c analyzers, and found that three of them did not meet generally accepted analytical performance criteria.7
In order to receive certification from the NGSP, HbA1c diagnostic methods must be traceable to reference values established by the Diabetes Control and Complications Trial. Thus, all such methods are calibrated to an HbA1c result. But not all methods measure true HbA1c—that is, hemoglobin glycated at the N-terminal amino acid of the beta chain. Instead, some assays measure total glycated hemoglobin. Immunoassays and high-performance affinity chromatography using an affinity column are both in this category. Immunoassays do not typically measure glycated F, but in any case, minimal elevations in the F fraction would not have a major effect on test results.
The bigger issue with methods that measure total glycated hemoglobins is that they cannot detect the presence of variant hemoglobins. If a variant is present that affects red cell half-life, it will not be identified. Two recent papers point out that HbA1c methods that do not recognize variants, while giving analytically correct results, can give clinically inaccurate results if those variants have an effect on red blood cell survival.8,9
“At Grady, I am using a borate affinity method on the Trinity Biotech Primus analyzer,” says Dave Koch, PhD, professor of pathology and laboratory medicine at Emory University, and director of clinical chemistry, toxicology, and point-of-care testing at Grady Memorial Hospital, both in Atlanta. “It will measure the glycated hemoglobin precisely and accurately in samples with nearly any variant, which is good. But if the life span of the red blood is different than 120 days, a diagnosis of diabetes should not be made based on an HbA1c result.”
A multicenter evaluation of a sister product from Trinity Biotech, Jamestown, NY, the Premier Hb9210 analyzer, concluded that the analyzer has acceptable precision and correlates well to HbA1c analyzers currently used in clinical practice and to the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) reference method procedure. The researchers concluded that the instrument is suitable for clinical application in the analysis of HbA1c.10
Don Wiebe, PhD, associate professor of pathology and laboratory medicine at the University of Wisconsin School of Medicine and Public Health, and director of toxicology at the University of Wisconsin Hospital and Clinics, both in Madison, uses the Tosoh G7 HPLC ion-exchange method. “I want to be able to tell the doctors if their patient has a hemoglobin variant,” he says. “Many times, they are not aware.”
Because there is evidence to suggest that hemoglobin variants may affect red blood cell half-life—even in hemoglobin trait cases that are asymptomatic—it is worth considering how the presence of common hemoglobin variants may affect HbA1c interpretation. (See Table 1.)
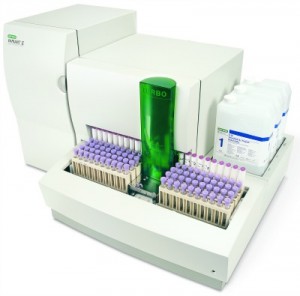
“The Bio-Rad Variant II Turbo has no interference from common hemoglobin traits, including S, C, D, and E,” says Scott Joksch, strategic accounts manager for the US sales division at Bio-Rad Laboratories, Hercules, Calif. “Physicians can be confident in knowing that a patient having a variant hemoglobin will be detected.” Joksch describes a project at Regional Medical Laboratories Inc, Tulsa, Okla, a lab that integrated its hematology line with HPLC HbA1c testing. The project was joint venture between Bio-Rad and IVD instrumentation manufacturer Sysmex, carried out at the Tulsa affiliate of Regional Medical Laboratories, Battle Creek, Mich.11
A relatively new technology among HbA1c assays is the Capillarys 2 Flex piercing A1c analyzer by Sebia Inc, Norcross, Ga. “The analyzer is based on capillary zone electrophoresis, and can analyze eight samples simultaneously for a throughput of 40 samples per hour,” says Aigars Brants, PhD, scientific affairs manager at Sebia. The instrument has been certified by IFCC and NGSP, and accurately measures true HbA1c. “The technology is also capable of performing complete hemoglobinopathy profiles with high accuracy and precision,” says Brants. Several peer-reviewed publications about the Sebia analyzer have recently appeared in the literature.12,13,14
REPORTING HbA1c
Considerable international effort has gone into standardizing HbA1c measurements and how they are reported. In the United States, most labs report HbA1c results in percentages only, whereas globally many labs report HbA1c results in Système International (SI) units (mmol/mol) only, or in both SI units and as percentages.
In 2007, an international consensus statement on the standardization of HbA1c measurement was published on behalf of the American Diabetes Association, the European Association for the Study of Diabetes, IFCC, and the International Diabetes Federation. This statement recommended that HbA1c results be reported worldwide in IFCC (SI) units and derived NGSP units (%).
While such a change would be easy to implement in most of the world, where SI units are already in place, it would be an expensive and confusing undertaking for labs in the United States. Thus, although implementing the change would make sense scientifically, after 10 years of debate over the concept, it still seems unlikely to happen in the United States.
“While it is widely known that the incidence of type 2 diabetes has dramatically increased among adolescents, there has also been an increase in the diagnosis of type 1 diabetes among adults into their 40s,” says Brian Feldman, MD, assistant professor of pediatrics at the Stanford School of Medicine, Stanford, Calif. “The detection of antibodies against one or more pancreatic islet antibodies (insulin, glutamic acid decarboxylate-GAD65, or tyrosine phosphate islet antigen 2) in a patient with hyperglycemia is diagnostic of type 1 diabetes and distinguishes the disease from type 2 diabetes,” says Feldman.
Presently, only radioimmunoassay (RIA) methods are available to assay the three antibodies. But Feldman and his research group at Stanford have developed a plasmonic chip for biomarker discovery and diagnosis of type 1 diabetes.15 Using a Licor Odyssey instrument to scan the chip, sensitivity and specificity are equal to the RIA methodology. “My goal is to develop an analytical platform that would be small and affordable, making the test available in a doctor’s office and ultimately in Third World countries,” says Feldman.
ADIPONECTIN LEVELS
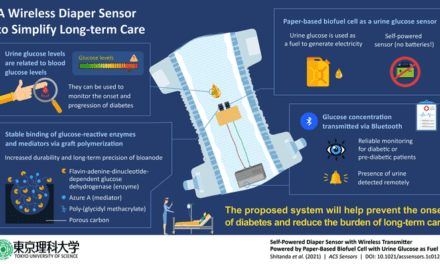
Testing adiponectin in the blood enables clinicians to assess a patient’s risk of developing type 2 diabetes and cardiovascular disease (CVD). Adiponectin is a protein hormone produced and secreted exclusively by adipocytes. It regulates the metabolism of lipids and glucose, and influences the body’s response to insulin. Adiponectin also has anti-inflammatory effects on the cells lining the walls of blood vessels. Low levels of adiponectin can be indicative of insulin resistance, leading to type 2 diabetes and CVD. Low adiponectin levels have also been shown to correlate with the increased likelihood of a woman developing gestational diabetes during pregnancy.
Using latex-enhanced immunoturbidimetric technology, Randox Laboratories Ltd, Crumlin, Co Antrim, UK, has brought a superior option for adiponectin assessment to laboratories, offering a biochemistry test instead of the more traditional and time-consuming ELISA-based testing,” says Louise McVicker, public relations executive at Randox.
“It is clear that in the 21st century, increasingly sedentary and desk-bound lifestyles are driving chronic conditions such as diabetes and cardiovascular disease,” says McVicker. “Across the world, 382 million people currently live with diabetes, and according to the International Diabetes Federation, this figure is predicted to rise by 55% by 2035.”
Adiponectin assesses an individual’s risk of developing diabetes, enabling “at-risk” individuals to make lifestyle changes in order to avoid or delay the onset of type 2 diabetes. “This highly targeted strategy should help to decrease the number of people becoming diabetic, enabling healthcare providers to save money and use resources more effectively,” says Pauline Armstrong, PhD, senior scientist at Randox Laboratories. The test is currently in clinical trials in Europe.
CONCLUSION
HbA1c is widely recognized as a valuable tool for assessing glycemic control in patients with diabetes, and it has more recently gained acceptance as a diagnostic tool. It is therefore very important that any unacceptable results are detected, and not reported. Each new method of measuring HbA1c levels must be evaluated for hemoglobin variant interference; no generalizations can be made based on method type.
When selecting an HbA1c assay method, laboratories should be aware of the limitations of the method and should consider the prevalence of hemoglobinopathies in their respective patient populations. In the presence of hemoglobin variants, assays that measure total glycated hemoglobin may report analytically correct results, but may not be clinically correct.
Craig C. Foreback, PhD, is a contributing writer and member of the CLP editorial advisory board. For further information, contact chief editor Steve Halasey via [email protected].
REFERENCES
1. Dabelea D, D’Agostno RB Jr, Mayer-Davis EJ, et al. Testing the accelerator hypothesis: body size, beta-cell function, and age at onset of type 1 (autoimmune) diabetes. Diabetes Care. 2006;29(2):290–294.
2. United States Renal Data System. USRDS 2007 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, Md: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, 2007. Available at: www.usrds.org/atlas07.aspx. Accessed October 16, 2014.
3. National Diabetes Statistics, 2007. Bethesda, Md: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, 2008. Available at: www.diabeteseducator.org/export/sites/aade/_resources/pdf/core_concepts/2007_NIDDK_DM_Statistics.pdf. Accessed October 16, 2014.
4. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2013;36(Suppl. 1):11–55.
5. Therapy for Diabetes Mellitus and Related Disorders. Alexandria, Va: American Diabetes Association, 2009.
6. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;3(Suppl. 1):S62–S69.
7. Lenters-Westra E, Slingerland RJ. Three of 7 hemoglobin A1c point-of-care instruments do not meet generally accepted analytical performance criteria. Clin Chem. 2014;60(8):1062–1072; doi: 10.1373/clinchem.2014.224311.
8. Rhea JM, Roberts-Wilson TK, Molinaro RJ. Impact of hemoglobin variants on HbA1c interpretation: Do we assume too much? Medical Laboratory Observer. 2012;44(6):8–14.
9. Rhea JM, Koch D, Ritchie J, et al. Unintended reporting of misleading HbA1c values when using assays incapable of detecting hemoglobin variants. Arch Pathol Lab Med. 2013;137: 1788–1791.
10. John WG, Little R, Sacha DB, et al. Multicentre evaluation of the Premier Hb9210 HbA1c analyzer. Clin Chem Lab Med. 2014:(Oct 2); doi: 10.1515/cclm-2014-0589. Epub ahead of print.
11. Patel N, Joksch S. Diagnostic testing in hematology: is it a solution for your lab? Medical Laboratory Observer. 2014;46(10):34–38.
12. Marinova M, Altinier S, Caldini S, et al. Multicenter evaluation of hemoglobin A1c assay on capillary electrophoresis. Clin Chim Acta. 2013;424:207–211; doi: 10.1016/j.cca.2013.06.014.
13. Jaisson J, Leroy N, Meurice J, et al. First evaluation of Capillarys 2 Flex Piercing (Sebia) as a new analyzer for HbA1c assay by capillary electrophoresis. Clin Chem Lab Med. 2012;50(10):1769–1775; doi: 10.1515/cclm-2012-0017.
14. Urrechaga E. High-resolution HbA(1c) separation and hemoglobinopathy detection with capillary electrophoresis. Am J Clin Pathol. 2012;138(3):448–456.
15. Zhang B, Kumar RB, Hongjie DH, et al. A plasmonic chip for biomarker discovery and diagnosis of type 1 diabetes. Nature Medicine. 2014;20:948–953.
16. McCurdy PR. 32-DFP and 51-Cr for measurement of red cell life span in abnormal hemoglobin syndromes. Blood. 1969;33(2):214–224.
17. Prindle KH, McCurdy PR. Red cell lifespan in hemoglobin C disorders (with special reference to hemoglobin C trait). Blood. 1970;36:14–19.
18. McCurdy PR, Mahmood L, Sherman AS. Red cell life span in sickle cell-hemoglobin C disease with a note about sickle cell-hemoglobin O ARAB. Blood. 1975;45(2):273–279.