Even though most big hospital laboratories don’t do their own billing, they still must enter correct billing codes for each procedure at the beginning of the process to ultimately be reimbursed for their services. These tasks must also be performed correctly by small, freestanding labs—which do their own coding, billing, and collections—so reimbursement can proceed quickly and accurately.
And although performing actual lab functions is handled routinely by software systems, LISs can also handle reimbursement from health insurance carriers and Medicare for the services laboratories perform. That’s a vital function because coding, billing, and reimbursement can be extremely time-consuming and labor-intensive, and, if payments are delayed, they can also create both customer and lab dissatisfaction. Therefore, a number of companies offer LISs that perform these functions while saving time, increasing efficiency, and freeing up lab personnel for other tasks.
STREAMLINING THE WORKFLOW
Starting with the inception of the order, it is imperative that correct billing information is not only presented on the claim, but also formatted based on the appropriate payor guidelines, says Gilbert Hakim, CEO of SCC Soft Computer, Clearwater, Fla. In tandem with the capture of the required information is automation of workflow processes due to the high-volume/low-dollar lab balances, he notes. “If billing and collection workflow becomes a manual process, then the labor component will quickly erode profit margins. This should be a mission-critical objective in the laboratory revenue cycle,” Hakim says.
Brian Keefe, marketing director, clinical products, Psyche Systems Corp, Milford, Mass, adds that billing and revenue cycle management is, as in any business, the lifeblood of the modern lab. Whether it is a hospital-based lab performing only inpatient work, mixed in with an outpatient/outreach business, or a small private lab or multiregional large reference lab, proper (or improper) handling of billing and coding will literally mean the difference between staying afloat or becoming a statistic.

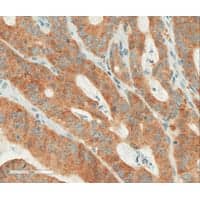
Orders can be placed in the EHR and sent electronically to LabDAQ LIS. When results are completed, they are sent to the EMR.
For Dianna Powell, presales clinical consultant, LIS, Merge Healthcare, Chicago, billing and coding are vital to the company’s clinical lab customers for two reasons: The sheer volume of work performed by most laboratories, as well as the multiple data elements required to properly bill for clinical laboratory tests, is substantive. “Each test or profile performed will consist of one or more separate billable items. Each billable item requires one or more diagnosis code, modifier, etc, along with the required demographic and insurance information specific to each patient,” Powell says. “Proper organization and submission of all this data is required to successfully bill for tests and receive optimal reimbursement for the laboratory work performed.”
Sandy Laughlin, LabDAQ product manager, Antek HealthWare, Reisterstown, Md, agrees that it’s very important for labs to bill and code correctly. “First, it’s key that a lab must remain profitable and receive accurate payment for testing that has been performed. Secondly, it’s important to ensure that the testing done and the diagnosis codes submitted with the procedure codes are part of the patient record.”
Laughlin says that in both large and small labs it is critical to capture the information correctly and ensure that the information gets into the billing software so services can be billed and payment received. Thus, there are often electronic interfaces in place between the LIS and practice management of billing software to ensure that all testing performed in the lab is captured in the billing software. Without the LIS/billing interface there’s a risk of missed billings because the testing is performed in the lab but not passed on to the billing software.
“It is often the lab’s responsibility to ensure that the proper diagnosis codes are provided prior to testing,” Laughlin says. Many LIS products have the ability to perform medical-necessity checking. With this checking, labs are alerted when the diagnosis code is not an acceptable code for reimbursement. “There are also tools in LIS systems to assist with testing frequency. The LIS will alert the user if the frequency limit for a particular test has failed.”
Labs, whether large or small, typically handle billing and coding in one of two ways, Keefe says. They either handle all billing internally with a specific billing/accounts receivable department staffed with coding professionals, or they rely on a growing trend toward outsourcing their billing/coding processes altogether. Many labs employ billing software systems, which can handle prescrubbing of lab orders for things like Medical Necessity/ICD-9 or ICD-10 correlations for Medicare, all the way through generating an actual invoice or bill.
A VARIETY OF APPROACHES
Different types of labs use different types of billing information systems, Keefe says. For example, many hospitals use their Hospital Information System (HIS) to process billing. Private and/or reference labs may employ a stand-alone/best-of-breed solution, which is interfaced to their LIS. Many LISs can accumulate and modify billing information during the processing of the lab work and subsequently send billing data across an interface to the billing system or company being used so that a complete bill can be generated, he adds.
Hospital-based labs and commercial labs approach this from different perspectives, Hakim says. Starting with hospital-based labs, they tend to leverage their current infrastructure—the HIS—to perform billing functions. This approach provides advantages while also creating disadvantages, he says. The convenience of using the HIS as the accounts receivable system is apparent from the minimal setup required to deploy what’s considered a “one-system” approach to billing and collections across all departments, he says.

The Merge LIS Order Entry screen is displaying a lab order that includes billing content. Diagnosis codes are associated with each procedure, and Merge LIS will generate an ABN for noncovered procedures.
However, “This one-size-fits-all approach looks attractive at first glance but does not provide the surgical precision expected from an accounts receivable system that is designed for the unique and fluid challenges of the laboratory industry. The HIS setup, which is geared for inpatient/outpatient billing, is not optimized for laboratory billing,” Hakim says. Functionality critical to the laboratory revenue cycle is prevention of late charges, payment/contractuals/denials posted to the test level, automation of tests bundling or exploding to components with modifiers based on payor guidelines, and laboratory financial drill-down reporting, he adds. Commercial laboratories share the same needs in critical functionality but also expect and require an accounts receivable platform that can track and trend reimbursement patterns against expected rates.
Hakim says SCC Soft Computer recognizes the challenge to integrate the front-end and back-end processes by using industry-inspired technology that is flexible, quick to deploy, and tightly integrated with the LIS and with automation built into every workflow. SCC’s Outreach Information Systems Suite of products—including SoftWebplus, SoftCompliance, and SoftA/R—is designed to deliver the critical functionality needed to meet the demands of the laboratory industry, he says.
IDENTIFYING KEY FACTORS
For Keefe, the main challenges posed by billing and coding are:
- Broad-scope changes in health care/Medicare law, which have negatively impacted the parameters used to calculate reimbursement for laboratory tests, resulting in drastically reduced payment by Medicare and private insurances for laboratory testing.
- Rapid adoption of practice management and electronic medical record (EMR) systems due to the American Recovery and Reinvestment Act’s HITECH Act’s Meaningful Use Initiatives to institute a universal EMR, which presents numerous challenges for labs that are tasked with interfacing to a wide range of disparate platforms with varying degrees of sophistication.
- Pressure to compete for business against other local or national laboratories requires technologies to support growth or the Outreach software solutions to deploy a seamless end-to-end integration with their provider clients.
- Rapid proliferation of new diagnostic testing methodologies, particularly in anatomic and molecular pathology labs, force labs to make a choice between high volume/lower reimbursement and low volume/higher reimbursement tests.
- Lack of integration/interfacing expertise, or limited functionality provided by the lab’s LIS or current billing solution vendor.
- Managing the varying insurance provider rules governing whether a lab is eligible to perform the testing if a patient has a particular insurance, or if it must send the work to a reference lab. Many labs can perform testing if it is ordered STAT, for example. Otherwise, they are faced with eating the cost of the work to keep a customer versus losing revenue to a competing laboratory by sending it out.
- Evolution of ICD-10 coding. Logical Observation Identifiers Names and Codes (LOINC) standard adoption are forcing labs to employ new coding standards by a certain date (within the next 12 to 24 months).
In both big and small labs, the challenges are similar; it is the scale that is different, Powell says. “Most lab managers want staff to touch the requisition or order only once,” she says. “Ideally, orders transmit from an EMR or are manually entered into the LIS. The most efficient workflow occurs when orders include all data required to properly bill for the work performed, and all of this necessary data is then transmitted to a billing system where it can be processed.”
THE RIGHT TOOL FOR THE JOB
Labs are asking for tools to assist with reimbursements and to make the lab more efficient, Laughlin says. “Connectivity with EHR and billing is also critical for the laboratory. Orders can be placed in the EHR and sent electronically to LabDAQ LIS. When results are completed, they are sent to the EMR.”
And laboratories are looking for specific reporting tools, complex billing logic for claim generation, automation of workflows, and transparency of operation, Hakim says, adding that another factor to consider is addressing the continuing change in regulatory requirements (for example, 5010 and ICD-10).
“Meeting these needs requires focus on business intelligence tools, customization to meet the unique needs of today’s clients, and continued commitment to provide innovative revenue cycle solutions. The expanded role of genetic testing as it relates to the laboratory industry is also driving new development,” Hakim says.
For Psyche, the most common request is options for integration to a third-party billing system or service provider. Other requests include:
- Rapid, efficient, and affordable integration to many different EMR and practice-management systems;
- Support of LOINC and ICD-10 coding standards;
- Integrated billing functionality within the LIS itself (not a separate module); and
- Ability to massage billing data using advanced rules prior to sending the billing info from the LIS or Outreach system.
Powell says labs, “particularly our physician office labs, are asking most about how they can qualify for ‘Meaningful Use’ dollars from the federal government. Merge is working closely with many existing and new EMR vendors, writing and deploying HL7 interfaces to support systems integration. Many of these integrations include orders transmitted from the EMR to the LIS, results transmitted from the LIS to the EMR, and charges transmitted from the LIS to the practice-management system, all of which help our Merge LIS customers qualify for ‘Meaningful Use’ reimbursements.”
Merge Healthcare offers the comprehensive Merge LIS. While not a billing system, Merge LIS does offer many billing and coding solutions for clinical laboratories that need a logical, organized, and easy-to-use LIS that translates the lab work performed into easily billable components. Merge LIS can perform medical-necessity checking, generate Medicare ABNs, associate billing modifiers with lab procedures, and more. These billable components can be electronically transmitted to a practice-management system or HIS via an HL7 billing interface or printed on a billing summary report for manual transcription by billing staff into the billing system. Merge LIS can even distinguish between lab procedures performed at a reference lab and those performed in-house, excluding from billing, any charges for direct third-party, or patient bill send-out orders, Powell says.
Psyche’s products support the laboratory’s overall billing and coding function, and also partner closely with billing and accounts receivable technology and service providers, Keefe says. “Our WindoPath Clinical & Anatomic Pathology Information System is able to accumulate billing information throughout the life cycle of specimen processing, and is able to support the latest integration standards for delivering that information in the required format to the AR/Coding system,” he says.
Psyche’s Outreach & EMR/PMS Integration Suite provides integration with EMR and PMS systems, which are the initial source of information used to create and issue a proper bill. PMS Bridging, EMR Interfacing, Medical Necessity Checking, and Rules-Based Insurance Provider Test Routing are all products and solutions Psyche offers to labs of all sizes and types that they can use to help achieve the highest return on investment on their laboratory testing services.
Antek HealthWare provides the LabDAQ Laboratory Information System, and its parent company, CompuGroup Medical, offers several practice-management systems—NetPractice PM and HPM, and Alteer office—Laughlin says.
Gary Tufel is a contributing writer for CLP.