Summary:
Natural disasters and the COVID-19 pandemic disrupted colorectal cancer (CRC) diagnoses in Puerto Rico, leading to a rise in late-stage cases due to delayed screenings.
Three Key Takeaways:
- CRC diagnoses sharply declined during and after Hurricanes Irma, Maria, and the COVID-19 lockdowns, likely due to disrupted healthcare access.
- Late-stage CRC cases eventually exceeded expectations, while early-stage diagnoses remained below expected levels.
- Researchers stress the need for more resilient healthcare systems to ensure continuity of care during crises.
Rates of colorectal cancer (CRC) diagnoses dropped during and shortly after Hurricanes Irma and Maria and the COVID-19 pandemic in Puerto Rico, according to a recent analysis. However, late-stage diagnoses eventually exceeded expectations, suggesting that limited access to cancer screening services due to these disasters likely hindered timely CRC diagnoses. The findings are published by Wiley online in CANCER, a peer-reviewed journal of the American Cancer Society.
Disasters May Delay Medical Services
During disasters, medical services may be delayed or inaccessible due to damaged infrastructure, overburdened health care facilities, or shortages of medical personnel. This can lead to late diagnoses, interruptions in treatment, and an overall worsening of survival and other health outcomes for patients.
To assess the impact of Hurricanes Irma and Maria and the COVID-19 lockdown restrictions on CRC diagnoses, investigators analyzed 2012–2021 data from the Puerto Rico Central Cancer Registry, which has been collecting information on all cancer cases diagnosed and treated in Puerto Rico since 1950.
The team led by investigators at the University of Puerto Rico found that from 2012–2021, a total of 18,537 residents received a first-time diagnosis of CRC. In the month the hurricanes struck, 161.4 CRC cases would have been expected in the absence of any interruption, but instead, only 82 cases were diagnosed.
After a slight upward trend, there was a second decline following the COVID-19 lockdown restrictions. In April 2020, the observed number of CRC cases was 50, but the expected number of cases without interruptions would have been 162.5.
Study Results Offered Unexpected Outcomes
By the end of the study, the estimated numbers of patients with early-stage CRC and those aged 50–75 years (the recommended screening age range) did not reach expected numbers. Meanwhile, numbers of patients with late-stage CRC and those outside the recommended screening age range (<50 years and ≥76 years) exceeded expected numbers.
“These findings suggest that limited health care access during these events may have delayed cancer detection and may have worsened health outcomes. This issue is especially critical in Puerto Rico, since the health care system already faces important challenges,” says co–lead author Tonatiuh Suárez-Ramos, MS. “Understanding these disruptions can help develop more adaptable and resilient strategies to ensure the continuity of essential care,” added co-lead author Yisel Pagán-Santana, DrPH.
Senior author Karen J. Ortiz-Ortiz, DrPH, stressed the urgent need for policies that strengthen health care systems in Puerto Rico and other regions that face similar challenges.
“By evaluating the impact of events like hurricanes and the COVID-19 pandemic, we hope to start the conversation about long-term solutions to improve cancer care coordination, reduce health disparities, and ensure continued access to care,” she says. “Ultimately, our goal is to help people live longer, healthier lives by making health care systems more resilient and accessible, even in times of crisis.”
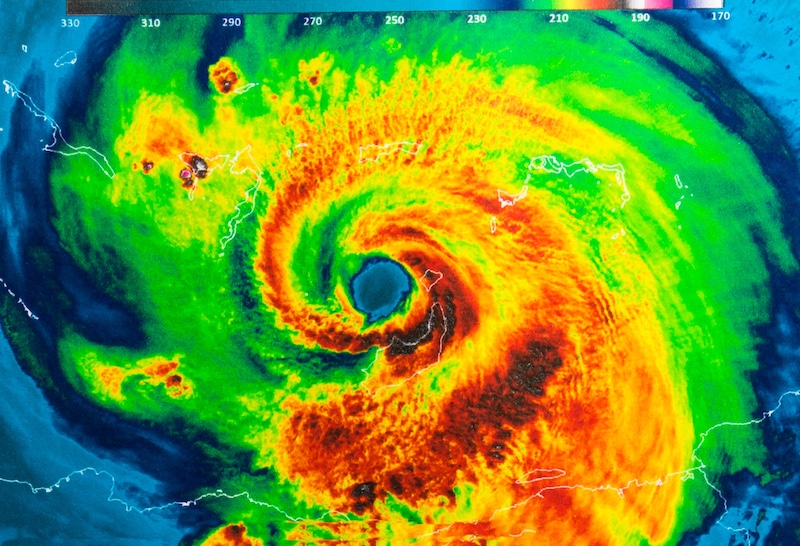
Featured Image: Trong Nguyen | Dreamstime.com