Traces of SARS-CoV-2, the virus that causes COVID, can be detected in microscopically small fluid breath droplets exhaled during a very short time span, a new study has found.
The findings came from the University of Gothenburg and have been published in the journal Influenza and Other Respiratory Viruses The measurement to determine results was carried out primarily with an advanced research instrument developed by the publishing research team.
The measurements were made with the research instrument Particles in Exhaled Air (PExA), developed at Occupational and Environmental Medicine at Sahlgrenska Academy, and with a smaller handheld instrument called the Breath Explor (BE).
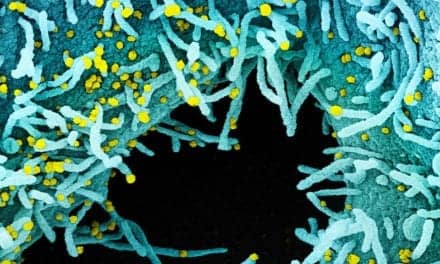
Researchers have shown that just a few breaths of exhaled air are sufficient for detecting traces of viruses in microscopically small fluid droplets (i.e. particles) exhaled from small airways, at least early in the course of a COVID-19 infection.
“We show that aerosol particles with the ribonucleic acid (RNA) virus can be found early in the course of COVID-19. The particles we can detect are very small–less than five micrometers in diameter–and we have here managed to capture particles with RNA virus in just a few breaths,” says Emilia Viklund, a doctoral student in occupational and environmental medicine and lead author of the study.
The findings may lead to assumptions about possibly replacing nasal swab tests, but professor Anna-Carin Olin, the inventor of PExA, suggests that would be extrapolating the findings too far.
“Respiratory viruses such as SARS-CoV-2 are likely to be concentrated mainly in the nose and throat, and it is easiest to take samples from that mucous membrane to detect the infection,” says Olin. “In contrast, the method of taking measurement in exhaled air is a very promising way of studying how the virus affects the small respiratory airways and how this effect changes during the course of the disease. Among other things, we are working on studies of post-COVID conditions using this method.”
In an initial small study involving only 10 subjects conducted in the autumn of 2020, only one of the samples using this methodology was found to be positive. The researchers believe this resulted from conducting measurements too late in the course of the disease. In collaboration with Sahlgrenska University Hospital, which allowed parallel measurement in connection with employees taking polymerase chain reaction (PCR) tests on the hospital grounds, the study eventually evolved to include more subjects in an earlier stage of the disease. These measurements were conducted in the spring of 2021 on medical professionals who had just submitted positive PCR samples for COVID-19.
Three different techniques were used to collect the samples: 20 normal breaths; a technique in which study subjects briefly hold their breath after a very deep exhalation; and a technique in which the study subject coughed three times into the instrument.
The research shows unsurprisingly that coughing generated the most positive breath samples collected with PExA (8 of 25), followed by deep breathing (3 of 25) and regular breathing (2 of 25). Two positive aerosol samples from normal respiration were also generated when collected with the instrument Breath Explor, although these came from individuals who were separate from the PExA findings with normal respiration.
“The quantity of aerosol particles we needed for the test was about one 10-millionth of the amount from nasal swab samples needed to detect viral RNA in regular respiration with PCR analysis,” says Olin. “The findings from the deep-breathing maneuver came as a surprise, the amount of sample is minute. Fluid droplets that one exhales after deep breathing form largely in the small airways, where it is known that the virus can cause great damage. As a result, it would be exciting to further study the findings in the exhaled air in relation to disease progression.”
Featured image: Traces of the SARS-CoV-2 virus detected in microscopically small fluid droplets exhaled with an instrument, developed by a research team at the University of Gothenburg. Photo: Agnes Viklund