Clinical labs struggle to match tests and testing strategies to the challenges of the covid-19 pandemic
By John Conroy
Ever since the botched rollout of testing for covid-19 earlier this year, the healthcare infrastructure in the United States has been struggling to catch up. The cascade of initial missteps is a case study in how not to handle a pandemic—one that continues to reverberate through the US clinical laboratory community.1
In January 2020, the Centers for Disease Control and Prevention (CDC) might have used the effective diagnostic tests that the World Health Organization eventually shipped to more than 60 countries. Instead, CDC opted to ramp up production of its own assay, sending the test kits to US public health laboratories at the beginning of February. But laboratories across the nation soon discovered that CDC’s reverse transcription polymerase chain reaction (RT-PCR) kits contained contaminated reagents that made the tests’ results unreliable.
Compounding the problem, CDC required hospitals to send samples to laboratories that then forwarded the results to CDC’s central lab in Atlanta. The resulting delay in getting diagnoses meant that the agency needed to limit availability of the test to recent travelers returning from China and people who had been in contact with an infected person—effectively causing health authorities to miss early covid-19 cases in both Washington and California.
The missteps have continued. In late May, CDC admitted that it has been combining molecular diagnostics and serology tests in its tallies of testing performed nationwide. That practice obscures the nation’s true testing capacity for covid-19 and could lead to skewing the positivity rate. CDC now says that it has corrected the problem, but states like Georgia, Pennsylvania, and Texas have reported doing the same thing.2
Ashish Jha, MD, MPH, professor of global health and director of the Harvard Global Health Institute, was aghast. “The viral testing is to understand how many people are getting infected, while antibody testing is like looking in the rearview mirror,” he said. “The two tests are totally different signals.”
How Many Tests Are Enough?
In April, Jha’s institute estimated that the United States would need to test 900,000 persons daily for covid-19 in order to fully track the spread of the disease and diagnose those suspected of having it. That estimate was based on the assumption that states would remain on lockdown until at least May 15, according to the institute.3
Meanwhile, another recent report published by the Safra Center for Ethics at Harvard University approximated that the United States would need to ramp up to more than 5 million tests per day by early June. Written by a team of experts in public health, economics, technology, and ethics, the Roadmap to Pandemic Resiliencesays that 20 million daily tests will be required by mid-summer in order to safely reopen the US economy.4
The report “lays out how massive testing plus contact tracing plus social isolation with strong social supports, or TTSI, can rebuild trust in our personal safety and the safety of those we love,” the authors write. “This will in turn support a renewal of mobility and mobilization of the economy.”
Social distancing alone will only extend the shutdown to an unacceptable length at great economic cost, according to the authors. “We can instead fully restart the economy by August through a program of massive investment in public health infrastructure, especially diagnostic and serological testing, combined with effective contact tracing-and-warning programs, and supported individual quarantine and/or isolation,” the authors write.
The TTSI method “will eventually need to reach a capacity to test 2% to 6% of the population per day,” or between 5 million and 20 million persons daily, according to the report. “Creating the complex supply and delivery chains required for testing at this scale will require a rapid coordination of business activity unprecedented since World War II,” the authors say. Although the TTSI program could cost $50 billion to $300 billion over 2 years, that amount is “dwarfed by the economic cost of continued collective quarantine of $100 to $350 billion a month.”
But experts from the University of Minnesota Center for Infectious Disease Research and Policy (CIDRAP) suggest that a specifically targeted approach to testing may be more effective than a broad-brush effort. “Pandemic messaging needs to move beyond ‘test, test, test’ mantras, as the current testing reality is complicated and depends on a cascade of interconnected factors and our approach must be strategic,” they write in a report released on May 20. A ‘smart approach’ to testing “requires the right infrastructure, right population to test, the right test, and the right application of test results before the right actions can be taken.”5
Among the authors’ major recommendations is the appointment by the secretary of Health and Human Services of a “blue-ribbon panel of national experts” that includes representatives from public health, clinical laboratories, medicine, laboratory testing R&D, marketing, product support, ethicists, legal scholars, and elected officials. The appointments should be made by July 1, 2020. The report also recommends that each state use a “smart testing framework” based on CDC guidelines to support “an infrastructure that provides the right test to the right person at the right time, with timely results allowing for actions that minimize illness, deaths, and transmission.”
CIDRAP says that optimal testing within this proposed framework will require several essential elements, among them materials, supplies, skilled labor, and instrument capacity. “The fragile interdependencies among elements in the cascade mean that one lacking element will reduce the number of tests that can be performed,” the authors write. The tests must also offer sensitivity to correctly identify persons with covid-19 or antibodies and specificity to correctly identify persons who do not have the disease or antibodies.
Diagnostics on the Way
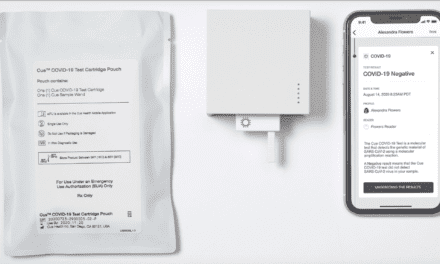
With varying degrees of success, reagent and equipment suppliers, in vitro diagnostics manufacturers, and laboratories are trying hard to meet this epochal challenge. In mid March, Quest Diagnostics, Secaucus, NJ, introduced a lab-developed test for covid-19 under an FDA emergency use authorization (EUA). The molecular test detects nucleic acid of SARS-CoV-2 in respiratory specimens. Quest said it was working with the American Clinical Laboratory Association to expand capacity. On May 28 Quest said it had received FDA EUA authorization for its self-collection kit, which allows users to collect their own nasal swab and ship the specimens overnight by FedEx at room temperature. The specimens can be tested using the Quest Diagnostics SARS-CoV-2 RT-PCR test launched in March.6,7
“Covid-19 molecular diagnostic testing has been constrained partly by limited supplies of swabs and trained healthcare professionals to do the specimen collection,” says Steve Rusckowski, president, chairman, and CEO, of Quest Diagnostics. “The self-collection kit enables an individual to self-collect at home, and the process is far less invasive and uncomfortable than many traditional methods.”
By the middle of May, Abbott Diagnostics had received EUAs for five covid-19 tests, according to John Hackett, divisional vice president for applied research and technology at Abbott. Another Abbott spokesperson noted that the company had already shipped more than 2 million molecular tests and more than 7 million antibody or serology tests to laboratories in the United States. The molecular tests can be performed on Abbott’s ID Now, m2000, or Alinity m instruments, while the antibody assays are performed on the company’s Architect system or Alinity i platform.8
“The pandemic has reminded us of the complex nature of diagnosing and treating patients, and the importance of collaboration,” says Hackett. “In this situation, industry is dealing with the added constraints of testing for a virus that we are learning more about each and every day.” According to Hackett, Abbott’s SARS-CoV-2 IgG serology assay has “greater than 99.6% specificity and 100% sensitivity, in patients tested 14 days after symptoms began.”
In mid-May, however, FDA issued an alert about Abbott’s molecular test, pointing to data that suggested “potential inaccurate results from using the Abbott ID Now point-of-care” test. The agency said it had received 15 “adverse event reports about the Abbott ID Now device that suggest some users are reporting inaccurate negative results.”9
FDA indicated that it is investigating whether the inaccurate test results might be caused by the types of swabs or the viral transport media used. Abbott said it will conduct postmarket studies for ID Now. At least 150 patients with positive covid-19 diagnoses in a variety of clinical settings will be included in the studies, and FDA will continue to review interim data.
Serology Missteps
Also in mid-May, Becton Dickinson announced that it would stop selling a point-of-care serological test made by BioMedomics, Morrisville, NC—one of around 100 ‘self-validated’ tests that flooded the market after FDA issued its EUA proclamation in mid-March.10The agency revised its policy on May 4 after many of the tests proved to be inaccurate. The new policy requires serological test manufacturers to submit EUA requests with validation data within 10 business days from the date they notify the agency of their validation testing.11
Meanwhile, CDC recently posted interim guidelines on the use of serological tests, acknowledging that most of the people in the United States have probably not developed covid-19 antibodies.12
“In most of the country, including areas that have been heavily impacted, the prevalence of SARS-CoV-2 antibody is expected to be low, ranging from less than 5% to 25%,” CDC says, “so that testing at this point might result in relatively more false-positive results and fewer false-negative results.” Because of the low prevalence of antibodies in most of the US population, “maximizing specificity, and thus positive predictive value in a serologic algorithm, is preferred in most instances.”
Well-known clinical lab and quality systems consultancy Westgard QC, Madison, Wis, cautions that laboratories face three risks in serology testing. The first is that not all of the tests with FDA emergency use authorization will perform as reliably as others. The second risk arises from the introduction of new diagnostic methods in serology tests submitted to FDA for an EUA. Unknown factors that occur during actual clinical use could produce inaccurate readings that would be discovered only later. A third risk arises from the nationwide dearth of the supplies needed by clinical laboratory customers to perform testing, according to Westgard.
Getting Paid
Many clinical laboratories have experienced a significant loss of income as a result of cutbacks in routine lab testing during the pandemic lockdowns that began in March. According to some analysts, labs may be positioned to recover some of their lost revenue by offering serology testing for covid-19.13
The Centers for Medicare and Medicaid Services recently announced a reimbursement rate of $42.13 for the most commonly performed covid-19 serologic tests at US laboratories.14Julie Khani, president of the American Clinical Lab Association, Washington, DC, praised the CMS decision, saying that the rate “will rapidly scale-up capacity for accurate and reliable serologic testing for SARS-CoV-2.” Commercial, public, academic, and hospital laboratories must all expand their capacity, Khani says.
“The announcement also reflects one of the important lessons learned from the rollout of covid-19 molecular tests,” Khani says. “We know that the lack of sufficient reimbursement for tests performed was a barrier to entry for many laboratories, and we have seen the positive outcomes from increasing the Medicare reimbursement rate for the molecular test.”
The CMS rate will enable laboratories across the United States to bring on additional platforms “to increase testing for high-risk populations, such as nursing home residents,” Khani says. But “robust federal funding” will be required so that all patients “regardless of insurance status have access to accurate and reliable serologic and molecular tests,” she adds.
Continuing Challenges
Irwin Redlener, MD, a clinical professor of health policy and management and pediatrics, and director of the national center for disaster preparedness at Columbia University, is scathing in his assessment of the testing debacle. “We started out on this whole question of testing with the CDC thinking about it as early as January and then into February and March,” he says. The overall approach “has uncovered some very inexplicable and surprising incompetence” and an inability to produce “crucially needed technology in a hurry. That remains true.”
FDA is looking at “400 different kinds of tests,” most of them diagnostic and some serologic, Redlener says. “We have so many continuing problems and challenges. Even highly touted kits like Abbott’s that the president was so excited about some weeks ago—it turns out some people think the accuracy is limited, even down to 50%. So it’s basically a coin toss.”
The United States needs “accurate, reliable onsite testing in order to open business,” Redlener says. Testing was first needed “to get a handle on the disease” in order to prevent it, and then to “allow the modelers to do some projections to be as prepared as we could possibly be.” Another key testing function was to enable clinicians to make rapid diagnosis of patients, he says.
Redlener says that opening local economies requires accurate testing in order to determine whether, for instance, the barber or the wait staff at a restaurant are negative or positive. That would require some form of testing every single day at the beginning of a shift, “so you’d feel comfortable taking your family to dinner, provided the restaurant followed other protocols such as separation of tables,” Redlener says.
“To me, testing has become the absolute key to the reopening of economies, which every state is trying to do in one form or another,” Redlener adds. “The absence of testing is a calamity that really should be a reason to pause in the mad rush to get the economy going. I’m deeply concerned about unemployment and the economy. It’s very, very bad. But I issue a stern caution about getting ahead of ourselves.”
John Conroy is a freelance writer based in Los Angeles.
REFERENCES
- Shear MD, Goodnough A, Kaplan S, Fink S, Thomas K, Weiland N. The lost month: how a failure to test blinded the US to covid-19 [online]. The New York Times.Updated April 1, 2020. Available at: www.nytimes.com/2020/03/28/us/testing-coronavirus-pandemic.html. Accessed May 30, 2020.
- Madrigal AC, Meyer R. ‘How could the CDC make that mistake?’ The Atlantic. May 21, 2020. Available at: www.theatlantic.com/health/archive/2020/05/cdc-and-states-are-misreporting-covid-19-test-data-pennsylvania-georgia-texas/611935. Accessed May 30, 2020.
- Begley S. Many states are far short of covid-19 testing levels needed for safe reopening, new analysis shows [online]. Stat. April 27, 2020. Available at: www.statnews.com/2020/04/27/coronavirus-many-states-short-of-testing-levels-needed-for-safe-reopening. Accessed May 30, 2020.
- Allen D, Block S, Cohen J, et al. Roadmap to Pandemic Resilience: Massive Scale Testing, Tracing, and Supported Isolation (TTSI) as the Path to Pandemic Resilience for a Free Society[online]. Cambridge, Mass: Edmond J. Safra Center for Ethics, Harvard University, 2020. Available at: https://ethics.harvard.edu/files/center-for-ethics/files/roadmaptopandemicresilience_updated_4.20.20_0.pdf. Accessed May 30, 2020.
- Ulrich A, Bartkus J, Moore KA, et al. Covid-19: The CIDRAP Viewpoint; Part 3, Smart Testing for Covid-19 Virus and Antibodies [online]. Minneapolis: Center for Infectious Disease Research and Policy, University of Minnesota, 2020. Available at: www.cidrap.umn.edu/sites/default/files/public/downloads/cidrap-covid19-viewpoint-part3.pdf. Accessed May 30, 2020.
- Quest Diagnostics launches coronavirus disease 2019 (covid-19) test [press release, online]. Clinical Lab Products. March 9, 2020. Available at: www.clpmag.com/2020/03/quest-diagnostics-launches-coronavirus-disease-2019-covid-19-test. Accessed May 30, 2020.
- FDA authorizes Quest Diagnostics covid-19 nasal specimen self-collection kit for emergency use [press release, online]. Secaucus, NJ: Quest Diagnostics, 2020. Available at: https://newsroom.questdiagnostics.com/2020-05-28-fda-authorizes-quest-diagnostics-covid-19-nasal-specimen-self-collection-kit-for-emergency-use. Accessed May 30, 2020.
- Our contributions to the covid-19 response [online]. Abbott Park, Ill: Abbott, 2020. Available at: www.abbott.com/coronavirus.html. Accessed May 30, 2020.
- FDA informs public about possible accuracy concerns with Abbott ID Now point-of-care-test [press release, online]. Clinical Lab Products.May 15, 2020. Available at: www.clpmag.com/2020/05/fda-informs-public-possible-accuracy-concerns-abbott-id-now-point-care-test. Accessed May 30, 2020.
- Crotti N. BD stops selling covid-19 antibody test it touted in March [online]. Mass Device. May 11, 2020. Available at: www.massdevice.com/breaking-bd-stops-selling-covid-19-antibody-test-it-touted-in-march. Accessed May 30, 2020.
- Shah A, Shuren J. Insight into FDA’s revised policy on antibody tests: prioritizing access and accuracy [press release, online]. Silver Spring, Md: FDA, 2020. Available at: www.fda.gov/news-events/fda-voices/insight-fdas-revised-policy-antibody-tests-prioritizing-access-and-accuracy. Accessed May 30, 2020.
- Using antibody tests for covid-19 [online]. Atlanta: Centers for Disease Control and Prevention, 2020. Available at: www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests.html. Accessed May 30, 2020.
- McBride M. With so many new covid-19 serology tests obtaining EUAs from the FDA, how can clinical laboratories identify tests that should perform reliably? Dark Daily[online]. May 20, 2020. Available at: www.darkdaily.com/with-so-many-new-covid-19-serology-tests-obtaining-euas-from-the-fda-how-can-clinical-laboratories-identify-tests-that-should-perform-reliably. Accessed May 30, 2020.
- LaPointe J. CMS releases Medicare payment rates for covid-19 test CPT codes. RevCycleIntelligence [online]. June 1, 2020. Available at: https://revcycleintelligence.com/news/cms-releases-medicare-payment-rates-for-covid-19-test-cpt-codes. Accessed June 1, 2020.
Featured image:
Colorized scanning electron micrograph of an apoptotic cell (green) infected with SARS-COV-2 virus particles (orange), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID.