Hospital-acquired infections exact a staggering toll, but new diagnostics help meet the challenge.
 |
One of the most common complications of hospital care, hospital-acquired infections are among the most insidious and challenging to eradicate. The Centers for Disease Control and Prevention (CDC) estimates that approximately 1.7 million hospital-acquired infections occurred in US hospitals in 2002 and were associated with 99,000 deaths. In addition to the tremendous toll on human life, the financial burden attributed to these infections is staggering, adding as much as $20 billion to health care costs each year.
Stepping up to the plate to help prevent these infections, the US Department of Health and Human Services unveiled a plan in January of this year that establishes a set of 5-year national prevention targets to reduce and possibly eliminate health care-associated infections. Also, two consortiums were formed last year to establish connections between hospital labs and leading academic labs to track drug-resistant patterns and new multiple antibiotic-resistant strains.
New Products on the Market for C. difficile
Prodesse Inc, Waukesha, Wis; BD Diagnostics, of Becton, Dickinson and Co, Franklin Lakes, NJ; and Cepheid, Sunnyvale, Calif, recently received clearance from the FDA to market products that diagnose Clostridium difficile, or C. difficile. The bacterium, found in the intestines, can cause severe diarrhea and life-threatening intestinal conditions, such as pseudomembranous colitis (inflammation of the large intestine), toxic megacolon (extreme inflammation and distention of the colon), and sepsis (a condition in which the body fights a severe infection that has spread via the bloodstream).
According to the CDC, C. difficile is a common cause of infectious health care-associated or antibiotic-associated diarrhea, accounting for 15% to 25% of hospitalized patients with antibiotic-associated diarrhea. Annually, there are more than 500,000 infections and more than 28,000 deaths in the United States, and more than 800,000 infections in the European Union. A recent national survey conducted by the Association for Professionals in Infection Control and Epidemiology suggests that 13 out of every 1,000 hospitalized patients are suffering from C. difficile, and more than 7,000 patients in US hospitals have the infection on any given day.
In addition, the average length of stay for a patient is nearly three times longer than the typical patient, and C. difficile is estimated to lead to $1 billion in excess health care costs annually in the United States or up to $51.5 million per day. The rates continue to increase, driven by a new epidemic strain known as BI/NAP1/027, which has now been detected in at least 38 US states, Canada, and 14 European countries.
The Health Protection Agency in the United Kingdom, which tracks deaths from C. difficile, reports that it is responsible for more deaths than the more widely known methicillin-resistant Staphylococcus aureus (MRSA), and that the death rate is increasing.
Many health care professionals maintain that the problem is compounded by the fact that more than 90% of US laboratories use immunoassay tests, which have been shown to be insensitive, with some testing below 50% compared to molecular testing. Even the gold standard cytotoxin test is reported to be only about 70% sensitive compared to molecular testing. In addition, the cytotoxin test is technically demanding and takes at least 2 days to produce results. According to Andy Shrago, senior vice president of sales and chief marketing officer at Prodesse Inc, some would even argue that the gold standard should be culture followed by the cytotoxin test, a procedure that takes even more time to produce results—time during which the infection goes untreated and can spread throughout the hospital.
The new tests may facilitate earlier and more appropriate antibiotic treatment of C. difficile patients. They may also lead to earlier implementation of infection control interventions that help prevent the transmission of the pathogen to other patients.
“Until molecular testing products, there was no way to get a fast, accurate answer to the question: Does this person have C. difficile?” Shrago says.
In April of this year, Prodesse received approval from the FDA to sell its diagnostic ProGastro Cd, which detects toxic strains of C. difficile. The tool uses real-time polymerase chain reaction (PCR) technology to produce a sensitive result on a stool sample in about 3 hours. Simple to use and with low inhibition, ProGastro Cd runs on a standard molecular instrument and fits easily into existing workflow, according to Shrago.
In trials at three clinics, ProGastro Cd detected 43% more positives than did the current gold standard. Genetic sequencing confirmed that more than 90% of the additional positives detected by ProGastro Cd were accurate. In addition, the three clinical sites reported no inhibited samples—an important aspect because stools usually have a lot of PCR inhibitors.
In January of this year, BD Diagnostics received the FDA go-ahead to market GeneOhm™—a molecular assay for the rapid detection of the Toxin B gene found in C. difficile.
According to Beth Billyard, senior product manager, GeneOhm was the first diagnostic that offered sensitivity, simplicity, and speed in one test procedure.
“The BD GeneOhm C. difficile assay provides a simple and rapid stool test with excellent sensitivity and specificity that allows same-day identification of toxigenic C. diff,” Billyard says.
“This test should improve patient care because it gives labs the option of a single assay that will markedly reduce or even eliminate the need for multiple screening and confirmatory tests,” she says. “This speeds up reporting and helps avoid unnecessary antibiotic use.”
According to Medical Director Tobi Karchmer, MD, before the advent of molecular testing, many physicians would ignore the results of the less sensitive tests if they didn’t confirm what the symptoms indicated.
“The clinicians would resend the test and order multiple tests,” Karchmer says. “They didn’t understand that ordering multiple tests using the same inaccurate method does not improve results. It doesn’t help and is costly.”
The GeneOhm assay targets the Toxin B gene, discovered in 1978 to be the cause of antibiotic-associated diarrhea and colitis and found in virtually all toxigenic C. difficile strains, including the emerging BI/NAP1/027 epidemic strain. It combines high sensitivity and specificity, and provides definitive test results in less than 2 hours.
Cepheid received FDA clearance in July for its Xpert® C. difficile test, the first on-demand molecular diagnostic test designed for 45-minute detection of the bacterium.
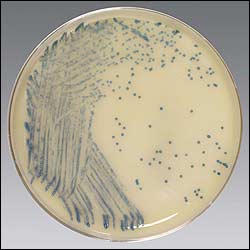 |
| Blue colonies represent a positive result for MRSA on the spectra plate. |
“The previous lack of an accurate and rapid diagnostic test for C. difficile has greatly impeded our ability to halt the increasing rate of C. difficile, which has taken a severe turn in the past several years. Patients can have their first diarrhea symptoms on a Monday and be dead by Thursday,” said Dale Gerding, MD, professor of medicine, division of infectious diseases, Loyola University Chicago Stritch School of Medicine.
“Toxigenic culture offers high sensitivity, but laboratories find it burdensome and far too slow for practical diagnostic use. Instead, many use less labor-intensive toxin EIA [enzyme immunoassay] and GDH [glutamate dehydrogenase] tests, which fail to detect 20 to 50 percent of cases,” he explains. “From a practical standpoint, this means many patients are not subjected to proper isolation procedures that can curtail transmission of C. difficile. A rapid, accurate test will eliminate needless repetitive testing and enable us to implement appropriate treatment and infection control measures faster in our battle against this devastating infection.”
The Xpert C. difficile test has been cleared for the direct detection of toxigenic C. difficile from stool specimens and targets the Toxin B gene. Cepheid will also continue to work closely with the FDA to deliver an additional product featuring simultaneous differentiation of the 027/NAP1/BI epidemic strain. The Xpert C. difficile test is Cepheid’s seventh test to receive FDA clearance, and fourth in its expanding menu of on-demand hospital-acquired infection products.
MRSA Remains Important Foe
While C. difficile may be challenging MRSA as the most widespread hospital-acquired infection, MRSA has certainly not gone away. The August 10/24 issue of Archives of Internal Medicine reports that MRSA appears relatively common among patients discharged from the hospital into home health care. In addition, about one-fifth of infected patients may transmit the organism to other people in their households.1
According to Carol Smith, senior product manager at Thermo Scientific, Remel Products, Lenexa, Kan, nasal MRSA colonization at admission or during hospitalization can increase the risk of MRSA infection. Once colonized with MRSA, 30% to 50% of patients become infected.2 In addition, while not all carriers will become infected, they could transmit the infection to other patients in the hospital, preventing effective public health control.
“Active surveillance for MRSA colonization is highly recommended for control of nosocomial transmission,” Smith says. “Rapid, accurate, and cost-effective screening tests for MRSA colonization are needed in order to reduce the economic burden of this pathogen.”
Remel’s Spectra™ MRSA is a selective and differential medium for detection of nasal colonization of MRSA. The test is performed with anterior nares swab specimens from patients and health care workers to screen for MRSA colonization.
An opaque medium, the product uses a novel chromogen that yields a denim blue color after 24 hours as a result of phosphatase activity. To allow the medium to differentiate MRSA accurately, it contains a combination of antibacterial compounds designed to inhibit the growth of a wide variety of competitor organisms. Also included are compounds that encourage the production of MRSA pathogenicity marker, ensuring expression of the phosphatase enzyme and so providing enhanced sensitivity and specificity. If after the 24-hour incubation no denim blue colonies are observed, the specimen is considered negative and plates should be discarded.
According to Smith, Spectra MRSA provides the highest positive predictive value compared to all other available methods, translating into lower false positives.
“With this excellent performance, hospitals can be assured that they are correctly identifying patients colonized with MRSA,” Smith says. “This allows appropriate patient isolation and contact precautions, and avoids the unnecessary financial burden of isolating or decolonizing a patient.”
The easy-to-use procedure and simple-to-read result allows for efficient batching on any shift in the microbiology lab. Results are available within 24 hours, regardless of positive or negative results. Additionally, no confirmatory testing is required for positives, which reduces ancillary testing and technician time in the microbiology lab.
BD Diagnostics also offers an assay for direct detection of nasal colonization by MRSA—the first on the market. The GeneOhm MRSA assay is a qualitative in vitro diagnostic test performed on the SmartCycler® instrument with a nasal swab specimen. It utilizes PCR for the amplification of MRSA DNA and fluorogenic target-specific hybridization probes for the detection of the amplified DNA. The GeneOhm MRSA assay is not intended to diagnose MRSA infections, nor to guide or monitor treatment for MRSA infections. Concomitant cultures are necessary only to recover organisms for epidemiological typing or for further susceptibility testing.
“From our assay, you do not have to do a culture confirmation,” Karchmer says. “The hospital could start an infection control based on the assay.”
Results can be obtained in 16 hours, a shorter time period than the chromogenic incubation period of 18 to 24 hours and far shorter than the 48 hours required to grow a culture.
Additional Pathogens Cause Almost 100,000 Deaths Per Year
Other hospital-acquired infections include myriad bloodstream infections, which can cause significant morbidity and mortality. According to the Infectious Diseases Society of America, every year, 350,000 patients contract bloodstream infections in US hospitals, causing more than 90,000 unnecessary deaths and significant costs to the health care system. Rapid and accurate identification of the specific infecting pathogen is thus crucial to ensure early and appropriate therapy and save patient lives, according to Will Harris, product manager of AdvanDx, Woburn, Mass.
In May, AdvanDx received FDA clearance for its EK/P. aeruginosa PNA Fluorescence In Situ Hybridization (FISH) test—the first diagnostic for identifying E. coli, K. pneumoniae, and P. aeruginosa directly from positive blood cultures. Patients afflicted by these infections spend an average of 5 to 24 days in the hospital, suffer mortality rates as high as 40%, and cost institutions on average $40,000 to $60,000 per case, according to the journal Clinical Infectious Diseases.3
These grim statistics are due in part to Gram-negative bacteria’s increasing resistance to a multitude of antibiotic agents, especially in P. aeruginosa and increasingly in K. pneumoniae, which creates complex therapy decisions for clinicians. Treatment challenges are further compounded by conventional laboratory testing methods, which take 24 to 48 hours or longer to identify the causative pathogen. This often forces clinicians either to treat patients unnecessarily with broad-spectrum antibiotics to cover the risk of resistant pathogens, or provide inadequate treatment if highly virulent and resistant pathogens are not suspected and treated.
AdvanDX’s new test provides critical results 24 to 48 hours sooner than conventional methods, with test results available within hours, instead of days, for 95% to 99% of all patients with bloodstream infections.
“This test helps labs to provide faster results, and allows physicians to make more informed treatment decisions early and improve patient care in hospitals and overall hospital operations,” Harris says.
Studies show that providing a 24-hour “head start” on appropriate narrow-spectrum therapy for Gram-negative bloodstream infections may improve clinical outcomes, reduce antibiotic resistance rates, and reduce the incidences of adverse events.
PNA FISH is an easy-to-use and highly sensitive and specific fluorescence in situ hybridization assay that uses peptide nucleic acid (PNA) probes to target species-specific ribosomal RNA (rRNA) in live bacteria and yeast. The unique properties of the noncharged, peptide backbone of PNA probes enable the use of FISH assays in exceedingly complex sample matrixes, such as blood and blood cultures, and this in turn facilitates the development of very simple, yet very accurate tests that don’t require the extensive sample preparation necessary for other nucleic acid technologies.
On the horizon is technology from the molecular diagnostic company Great Basin Scientific, Salt Lake City. The company’s technology is designed to improve the traditional methods of diagnostic testing of hospital-acquired infections, such as MRSA, allowing test results to come back in less than an hour versus the traditional 1- to 2-day waiting period.The results are a faster diagnosis and reduced patient hospital stay, which saves lives and money.

To stay current on autoimmune testing, bookmark our website. |
Great Basin Scientific’s silicon chip-based technology is simple, cost-effective, and improves on the highly complex, traditional PCR method that requires the skills of highly trained technicians and oftentimes multiple rooms to avoid cross contamination of tests. The company’s highly sensitive, easy-to-use integrated cartridge system, which can be performed in a CLIA-rated moderately complex or waived laboratory, will give health care providers and their patients the benefit of point-of-care test results within a 20- to 60-minute time frame at costs much lower than current molecular solutions. Clinical trials were expected to begin in August.
Shannon Rose is a freelance health and medical writer based in Temecula, Calif.
References
- Lucet JC, Paoletti X, Demontpion C, et al. Carriage of methicillin-resistant Staphylococcus aureus in home care settings. Arch Intern Med. 2009;169(15):1379-1380.
- Muto CA, Jernigan JA, Ostrowsky BE, et al. Infection control and hospital epidemiology. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and Enterococcus. Infect Control Hosp Epidemiol. 2003;24(5):362-386.
- Paterson DL. Impact of antibiotic resistance on gram-negative bacilli on empirical and definitive antibiotic therapy. Clin Infect Dis. 2008;47 Suppl 1:S14-S20.



