A study has revealed an entirely unexpected process for acquiring drug resistance that bypasses the need to reestablish DNA damage repair in breast cancers that have mutant BRCA1 or BRCA2 genes.1
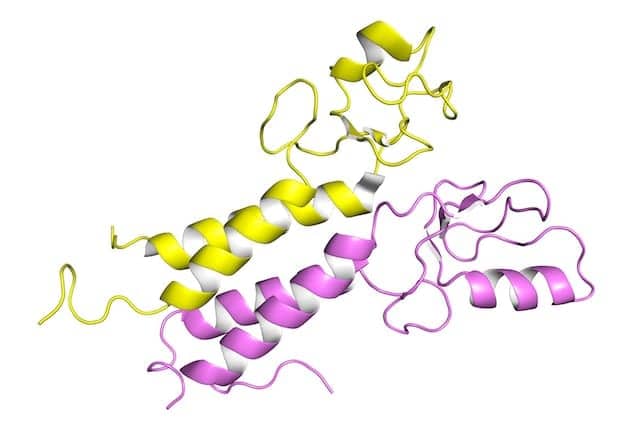
In normal cells, the proteins BRCA1 and BRCA2 act as DNA damage sensors, surveyors, and responders. They help perform complex functions that facilitate the repair of damaged DNA. Individuals who inherit certain mutations in either the BRCA1 or BRCA2 gene have defective DNA repair and an increased risk of developing breast, ovarian, and other cancers.
Specifically, mutations in BRCA1 and BRCA2 account for 20–25% of hereditary breast cancers and 5–10% of all breast cancers. The reduced ability of cells with a BRCA1 or BRCA2 mutation to repair breaks in DNA makes the cells sensitive to DNA-damaging drugs. However, breast cancers eventually acquire resistance to these drugs. One documented mechanism for developing chemoresistance in such tumors is through the restoration of accurate DNA repair pathways that mend DNA breaks caused by chemotherapy.
Researchers have spent the past decade trying to understand the cellular mechanisms that regulate DNA repair in normal and pathogenic states. “It is the intricate mechanisms that tumor cells evolve to bypass the need for accurate DNA repair that form the foundation of our study,” says study author Andre Nussenzweig, PhD. “A deeper knowledge of the processes that drive drug resistance in BRCA 1/2-mutant tumors will lead to novel therapeutic approaches that target tumor-specific vulnerabilities.”
In their study, the researchers linked the protection and stabilization of DNA replication forks as a major contributory mechanism to drug resistance in BRCA 1/2-mutant breast and ovarian cancers. Replication is a cellular process that produces two indistinguishable DNA copies from a single DNA molecule. This DNA-copying process is an essential step in cellular division and occurs at defined locations called replication forks.
The movement of a replication fork as it migrates along a DNA molecule can be disrupted by the presence of a diverse group of DNA structures and proteins, collectively referred to as replication fork barriers. This interruption of replication fork migration results in what is called a stalled fork. Upon replication fork stalling, the BRCA1 and BRCA2 proteins are called upon to protect the newly synthesized strands of DNA. If these proteins are absent, the replication fork is destabilized and the newly synthesized DNA is degraded, which increases genomic instability and increases sensitivity to DNA-damaging drugs.
The investigators were able to identify other proteins, such as CHD4, PARP1, and PTIP, that actively promote replication fork destabilization through the recruitment of enzymes that degrade newly synthesized DNA. The absence of these proteins protected the DNA at replication forks and remarkably reversed the drug sensitivity of both BRCA1- and BRCA2-mutant cells, making them chemoresistant.
The studies also highlighted the complex ways by which tumor cells can evade chemotherapeutic interventions and acquire drug resistance, since disrupting the activity of multiple proteins led to the same endpoint of replication fork protection. The results are of particular relevance in the clinical setting, where expression of these proteins appears to be an indicator of how patients with BRCA1- and BRCA2-mutant cancers will respond to chemotherapeutic treatment with DNA-damaging agents.
All together, the results underscore the importance of replication fork barriers to genomic instability and drug sensitivity in the context of BRCA 1/2 mutations. The results also suggest that the cellular levels of these proteins could be used as a prognostic factor in acquired resistance in BRCA 1/2-mutant cancers.
REFERENCE
- Chaudhuri AR, Callen E, Ding X, et al. Replication fork stability confers chemoresistance in BRCA-deficient cells. Nature. 2016;535(7612):382–387; doi: 10.1038/nature18325.