When a patient undergoes a surgical operation to remove a tumor or treat a disease, the course of surgery is often not predetermined. To decide how much tissue needs to be removed, surgeons must know more about the condition they are treating, including a tumor’s margins, its stage and whether a lesion is malignant or benign—determinations that often hinge upon collecting, analyzing, and diagnosing a disease while the patient is on the operating table. When surgeons send samples to a pathologist for examination, both speed and accuracy are of the essence. The current gold-standard approach for examining tissues often takes too long and a faster approach, which involves freezing tissue, can introduce artifacts that can complicate diagnostics. A new study by investigators from the Mahmood Lab at the Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, and collaborators from Bogazici University developed a better way; the method leverages artificial intelligence to translate between frozen sections and the gold-standard approach, improving the quality of images to increase the accuracy of rapid diagnostics and opening the possibility for real-time diagnoses during surgery. Findings are published in Nature Biomedical Engineering.
“We are using the power of artificial intelligence to address an age-old problem at the intersection of surgery and pathology,” says corresponding author Faisal Mahmood, PhD, of the Division of Computational Pathology at BWH. “Making a rapid diagnosis from frozen tissue samples is challenging and requires specialized training, but this kind of diagnosis is a critical step in caring for patients during surgery.”
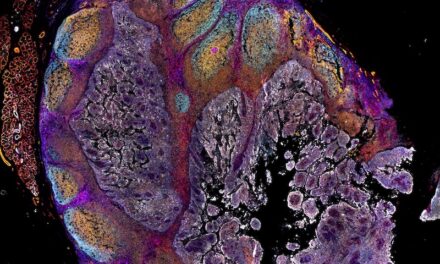
For making final diagnoses, pathologists use formalin-fixed and paraffin-embedded (FFPE) tissue samples—this method preserves tissue in a way that produces high-quality images but the process is laborious and typically takes 12 to 48 hours. For a rapid diagnosis, pathologists use an approach known as cryosectioning that involves fast freezing tissue, cutting sections, and observing these thin slices under a microscope. Cryosectioning takes minutes rather than hours but can distort cellular details and compromise or tear delicate tissue.
Mahmood and co-authors developed a deep-learning model that can be used to translate between frozen sections and more commonly used FFPE tissue. In their paper, the team demonstrated that the method could be used to subtype different kinds of cancer, including glioma and non-small-cell lung cancer. The team validated their findings by recruiting pathologists to a reader study in which they were asked to make a diagnosis from images that had gone through the AI method and traditional cryosectioning images. The AI method not only improved image quality but also improved diagnostic accuracy among experts. The algorithm was also tested on independently collected data from Turkey.
The authors note that in the future, prospective clinical studies should be conducted to validate the AI method and determine if it can contribute to diagnostic accuracy and surgical decision-making in real hospital settings.
“Our work shows that AI has the potential to make a time-sensitive, critical diagnosis easier and more accessible to pathologists,” said Mahmood. “And it could potentially be applied to any type of cancer surgery. It opens up many possibilities for improving diagnosis and patient care.”